This year, the Digital Health Summit (#DHS2022) was held at the Sydney International Convention Center (ICC) on 17-18 October 2022. The Summit, co-organized by the Australasian Institute of Digital Health (AIDH) and eHealth New South Wales (NSW), had a jammed packed variety of interesting talks and programs for its over 1000 delegates from all over Australia. Yes, there were some people from other countries, e.g. Toronto, UK and Singapore (aka me), but majority of the delegates travelled interstate to attend this conference.
Although there were many interesting tracks, the Summit was quite focused on a few topics – mainly in terms of health informatics, interoperability and addressing the workforce gap. There were a few sessions that I felt were interesting, and in my opinion, some of the approaches could be something that Singapore healthcare institutions/organizations could consider to adopt/adapt. My executive summary of my DHS experience is detailed as follows.
Telehealth & Virtual Care
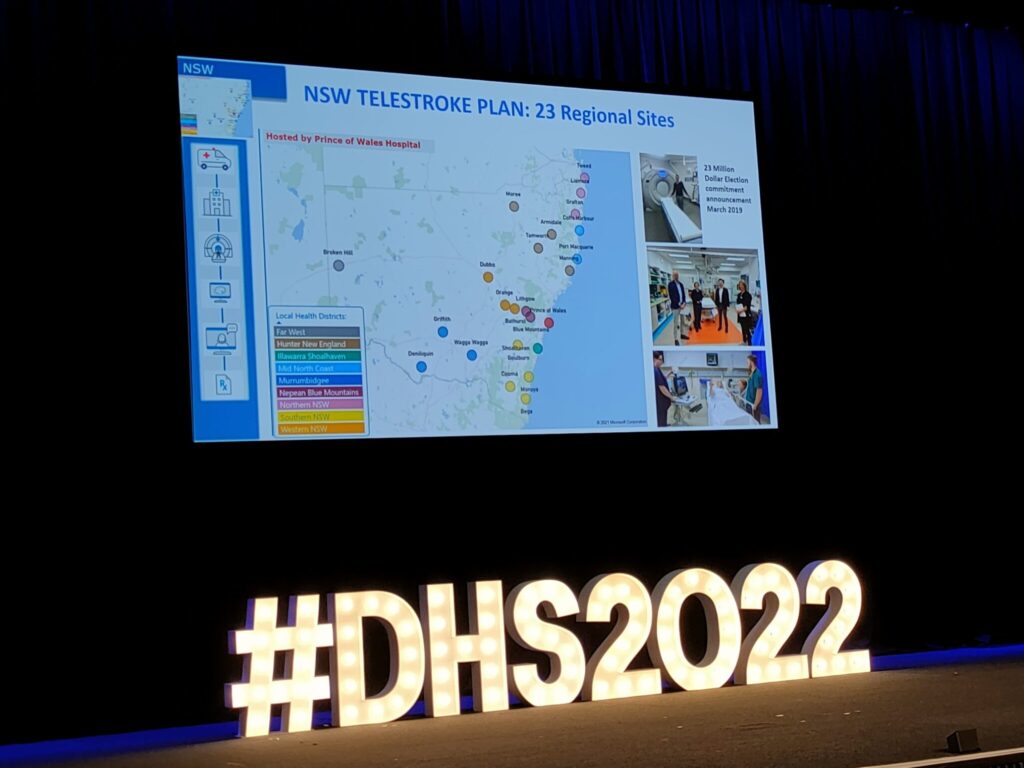
Unlike Singapore, telehealth services and mobile health (mHealth) applications really picked up in Australia during COVID-19. Many start-ups were seen in this area. Even the Australian Ministry of Health supported this digital health modality across various states and hospitals. For example, a NSW Telestroke Plan, hosted by the Prince of Wales Hospital, was implemented across 23 regional sites. Using a hub-and-spoke model of care combined with simple technologies (e.g. cart-on-wheels [COWs], webcams), cloud services (e.g. Amazon Web Services [AWS]) and familiar telecommunication applications (e.g. Microsoft Teams), patients who suffered from stroke could be triaged by a virtual doctor/neurologist to receive thrombolytic treatment, endovascular thrombectomy or be admitted to the stroke care unit. Of course, the clinical architecture was more complicated that I have just described, but this service had an impressive record of over 8,000 triage outomes, over 2,600 telestroke consultations and more than 500 reperfusion recommendations since its inception. Clinicians out there who want to know more about this telestroke service are referred to the BMJ Open publication.
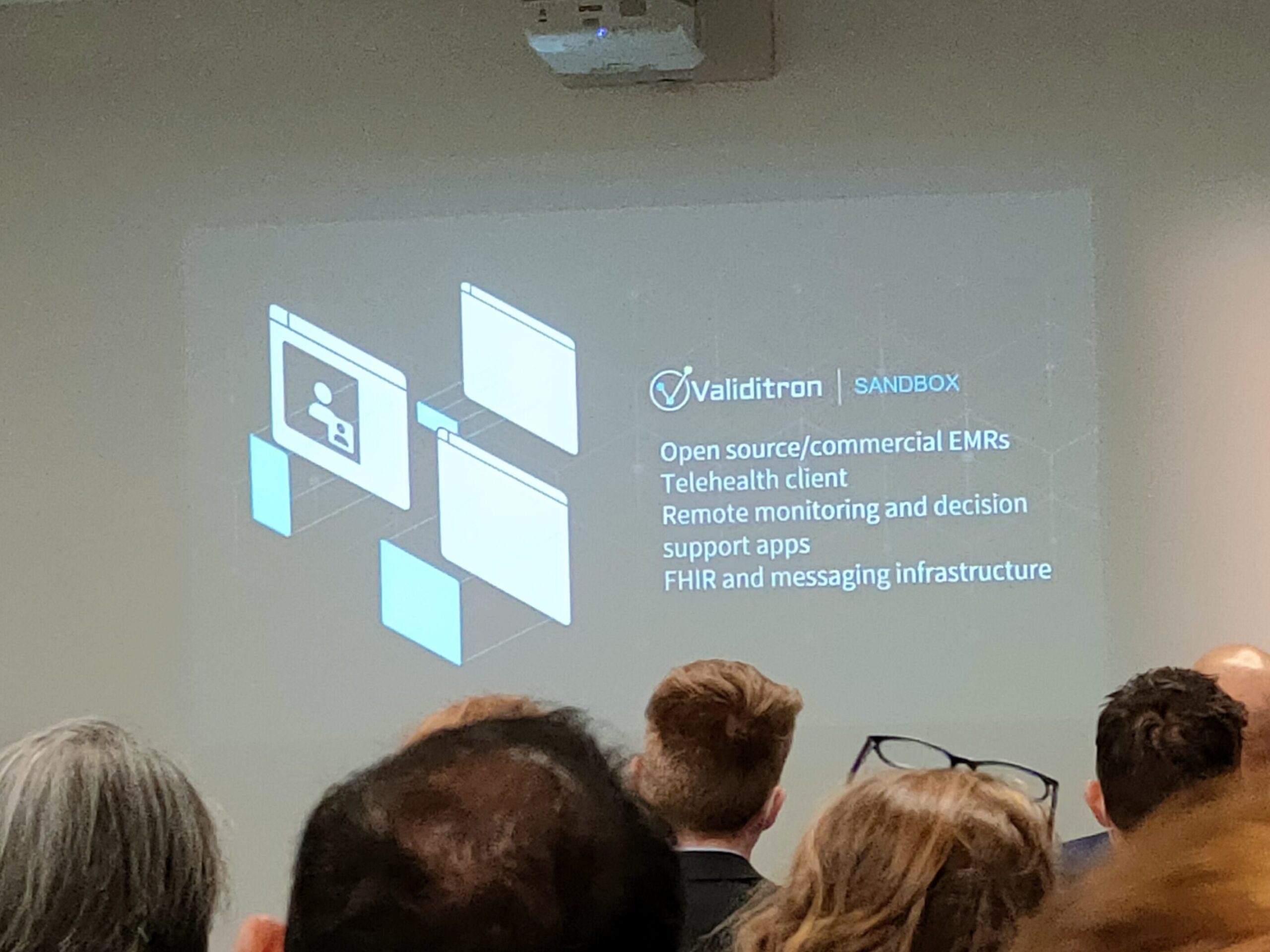
Validation Sandbox for Digital Health Innovations
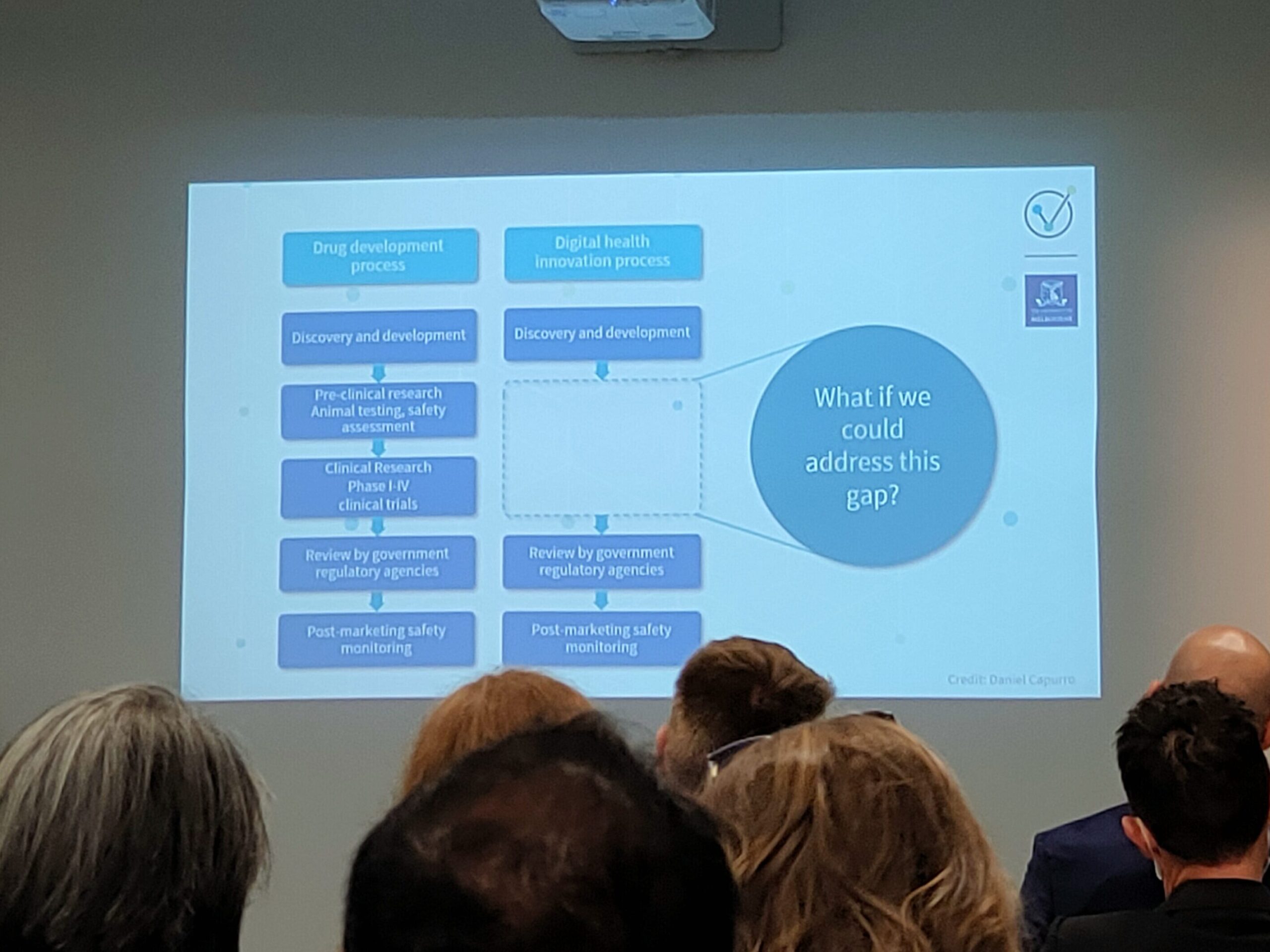
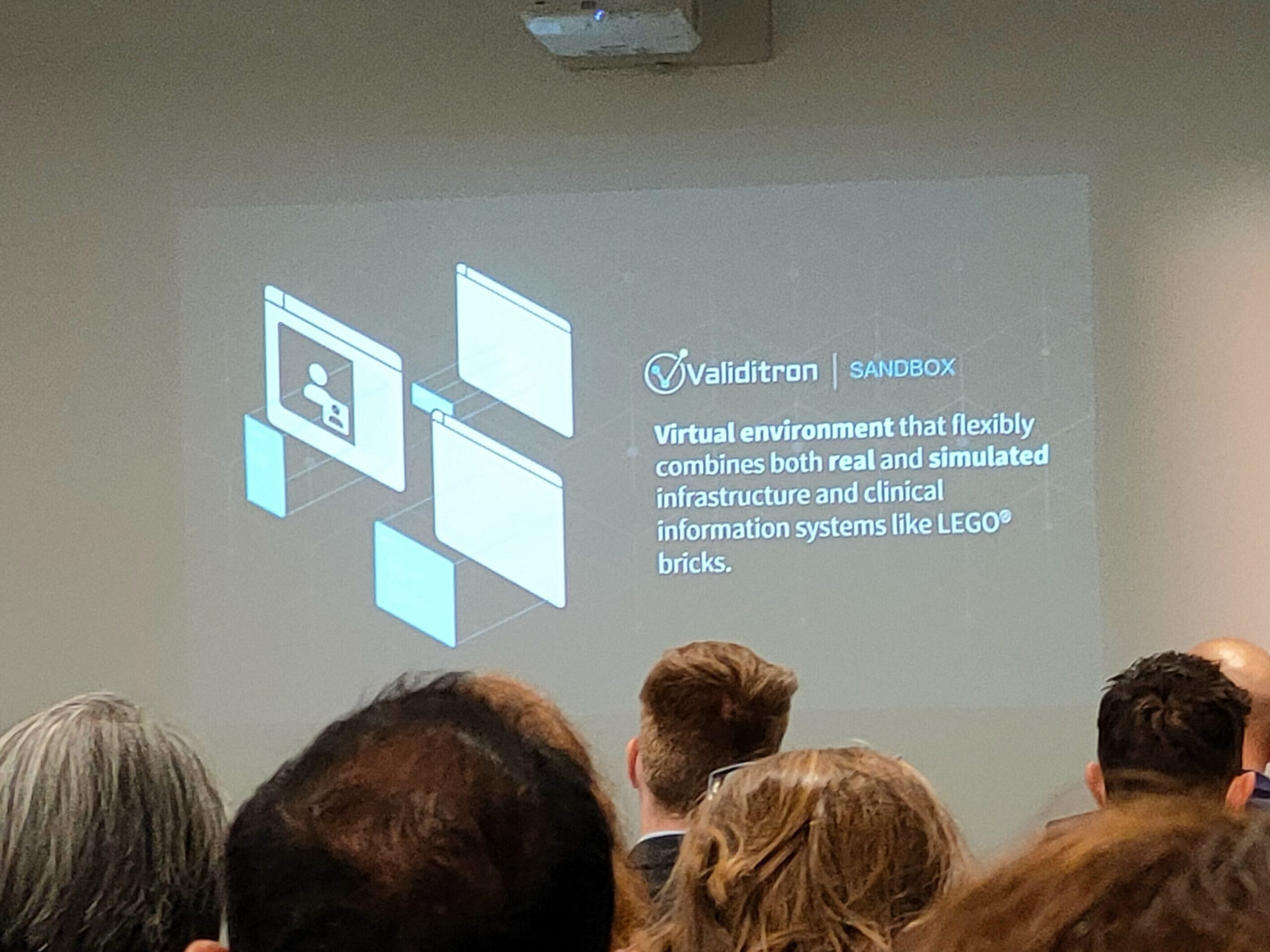
Dr Kit Huckvale, the Technical Lead for the Centre for Digital Transformation of Health at the University of Melbourne, talked about his “Digital Health Validitron” – a sandbox program to aid in successful design, development, validation and evaluation of digital health solutions. Unlike the traditional drug discovery and development process in which pre-clinical research and clinical trials are used to validate the efficacy of drugs, there is a gap missing in relation to determining the efficacy/effectiveness and safety of digital health innovations. His solution? A virtual sandbox environment – which he likened to Lego bricks – that is able to mimic clinical information systems and infrastructure to test electronic medical record (EMR) and virtual health applications.

Artificial Intelligence in Healthcare
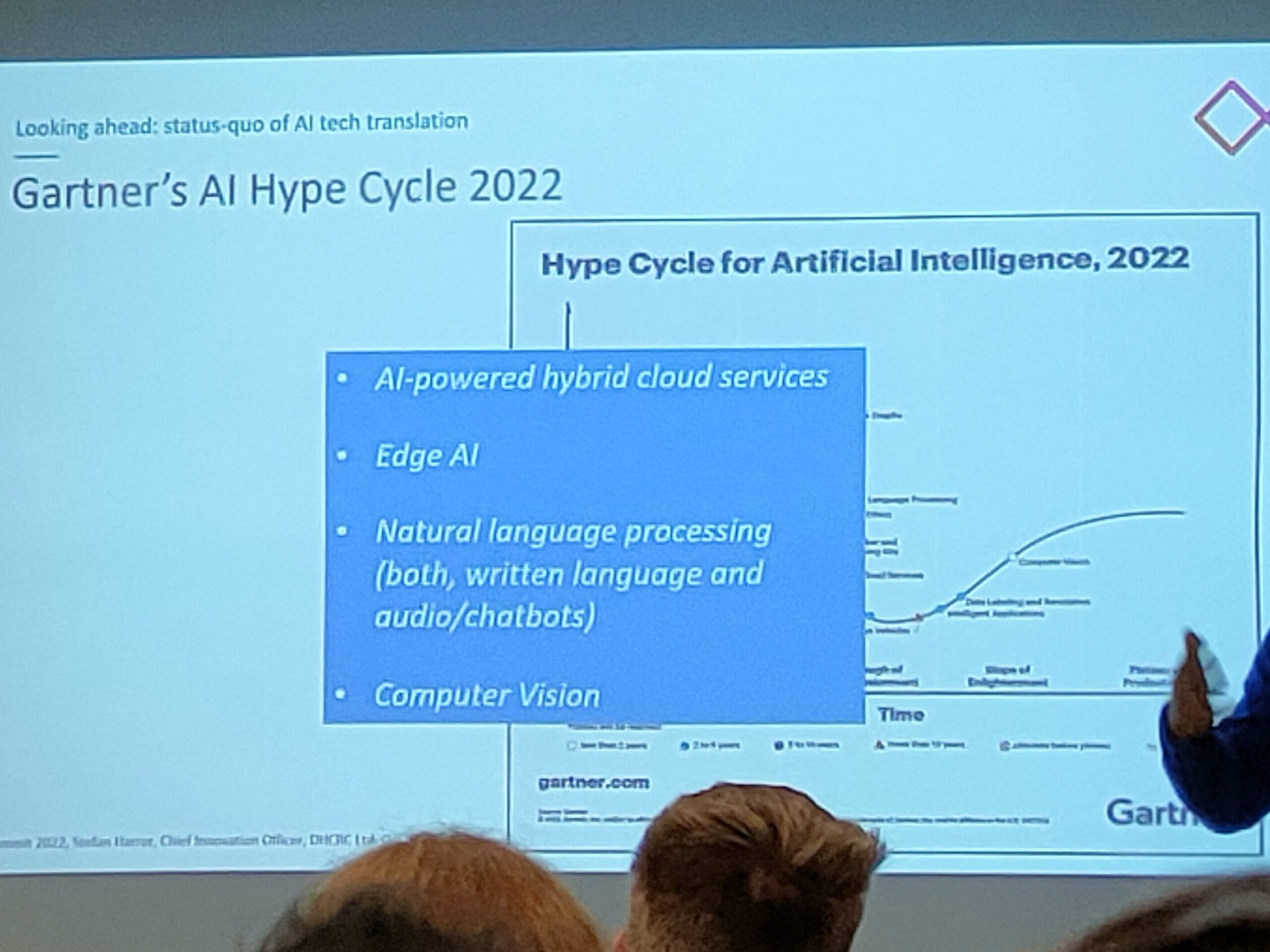
Artificial intelligence (AI) was in quite a number of presentations, though these presentations were running concurrently. I had to run around the various rooms to catch the topics in which I was interested in. Professor Stefan Harrer, Chief Innovation Officer of the Digital Health Cooperative Research Centre (DHCRC) talked about the topic on “You just heard ‘AI’, ‘data’ and ‘healthcare’ in one sentence: buzzword bingo or elevator pitch?” He emphasized that even though ‘AI’ was a buzzword, in healthcare, not everything is better with AI. In order to show that the AI application is relevant in healthcare settings, the application needs to have a clear value proposition for the use of AI, combined with consumer participation and endorsement, to show that it is solving a real-world problem. Through the Gartner’s AI Hype Cycle, he envisioned that the future of AI would lie in cloud services, edge AI, natural language processing, as well as computer vision.
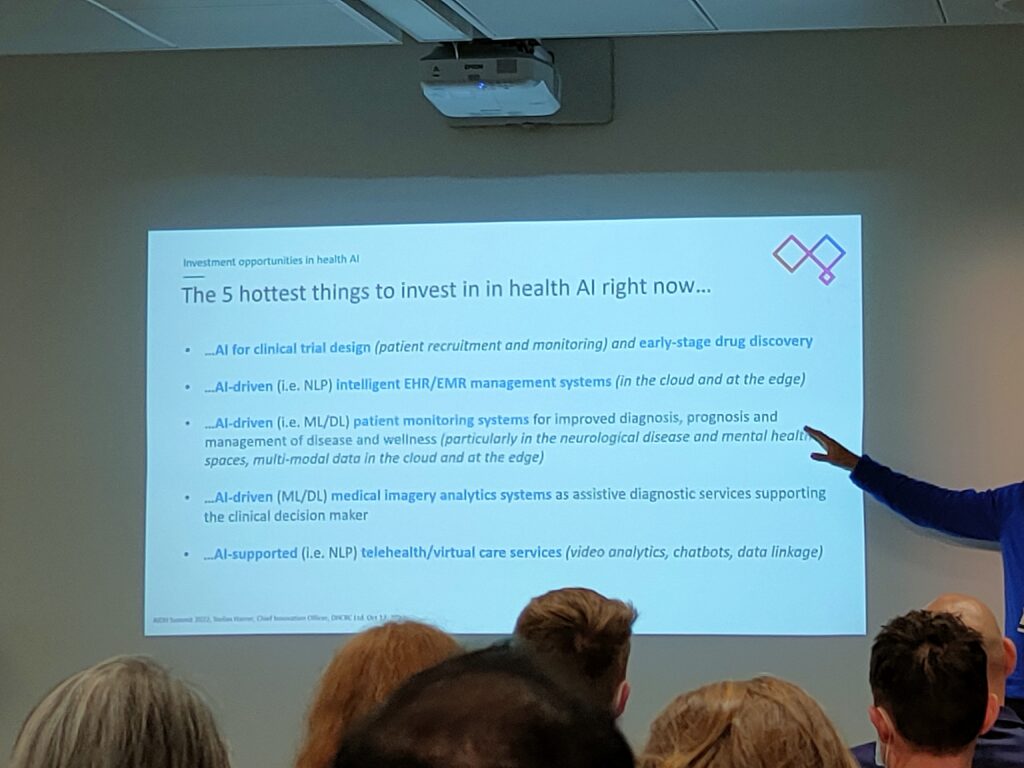
Prof. Harrer ended his presentation with what he thought would be the top investments in health AI. Within each category, I have also provided a non-exhaustive summary list of companies and application examples:
- AI for clinical trials:
- There are many AI-based clinical trial platforms springing up in the digital health arena. Some examples include Benevolent AI, Unlearn.AI, Deep Lens and AiCure, among others. In general, such AI systems aim to speed up the drug discovery process at its early stages by predicting optimal therapeutic leads for a wide range of diseases. At the other end of the spectrum, some clinical trial start-ups use their AI platforms to screen and match the Right patient with the Right trial at the Right time, while others provide real-time monitoring of patients to understand how they respond to the intervention therapy.
- AI-driven electronic medical/heath record (EMR/EHR) systems:
- For companies who offer AI-based solutions for EMRs/EHRs, these solutions generally comprise of a certain variety of functions – such as document searches, medical transcriptions and data analytics. For example, Linguamatics is a software company that uses natural language processing to visualize health-related data from EMRs/EHRs to clinician users (e.g. in the form of graphs and charts). On the other hand, Nuance Communications combines a voice recognition system and a machine learning algorithm in their natural language processing software (called Dragon Medical One) to enable clinicians to fill in health information into EMRs/EHRs by speaking into their computer microphones. The software will then transcribe the medical data from voice into the relevant section of the EMR/EHR. Through data analytics, AI can also be integrated with EMR/EHR databases to identify non-health-related data, such as patient satisfaction with their medical visits. For example, Cognizant has various case studies on how they have helped various healthcare organizations improve operations and service delivery by searching relevant reports, visualize trends and discover insights through their AI-based business analytics model.
- AI-driven patient monitoring systems:
- With the hospital bed-crunch accelerated during COVID-19, healthcare organizations are recognizing the value of “hospital-in-a-home”-based patient monitoring systems. And with advancements in wearable devices and biosensors, why not? Remote patient monitoring can lead to improved healthcare accessibility (especially to patients living in rural areas), better quality of care (since patients’ health parameters can be monitored by clinicians without physical visits), time and cost savings to patients (as they do not need to spend time and money travelling to the hospital/clinic), and potentially, better treatment adherence leading to better patient outcomes. Various companies have targeted this space of AI-based remote patient monitoring for conditions such as heart and respiratory diseases, through data insights from various technologies like electrocardiograms (e.g. Cardiologs , iRhythm), apps and wearables (e.g. Myia Health, Current Health), and even smart patches (e.g. ten3T Healthcare)!
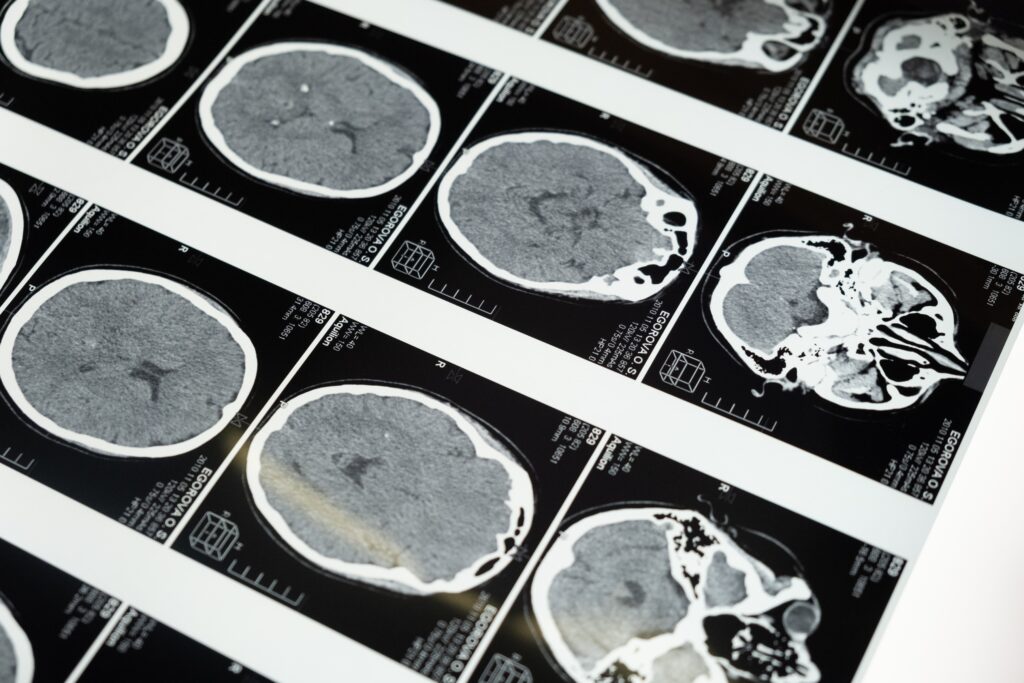
- AI-driven medical imaging and analytics:
- The aim of AI-driven medical imaging is to use machine learning and/or deep learning algorithms in imaging processing to identify specific patterns and anatomical markers to perform quick visualizations and diagnoses. Common applications for AI-based imaging include those for cancer detections, identification of cardiovascular abnormalities, neurological imaging, ultrasound imaging, and for surgical planning, among others. Besides IBM Watson, who was one of the pioneers in AI-based healthcare applications, there are now many other AI-driven medical imaging companies that have entered this field – such as Lunit, Arterys, Butterfly Network, Enlitic, Viz.ai, RetinAi and BrainMiner, etc.
- AI-supported telehealth and virtual care:
- Besides the examples that I have provided above (which are not totally segregated from telehealth and virtual care services), other technologies that can play towards AI-supported telehealth and virtual care include chatbots, data linkage and video analytics. The advantages of leveraging on AI in telehealth and virtual care are that AI can help in smart remote patient monitoring, provide better diagnoses, and potentially address the workforce challenges in the healthcare industry by reducing hectic administration tasks and streamlining/improving workflow processes. For example, Babylon and Ada have developed successful AI chatbots for patient triaging, while Amazon Alexa has been used by hospitals in the US as a conversational virtual assistant for patients and clinicians.
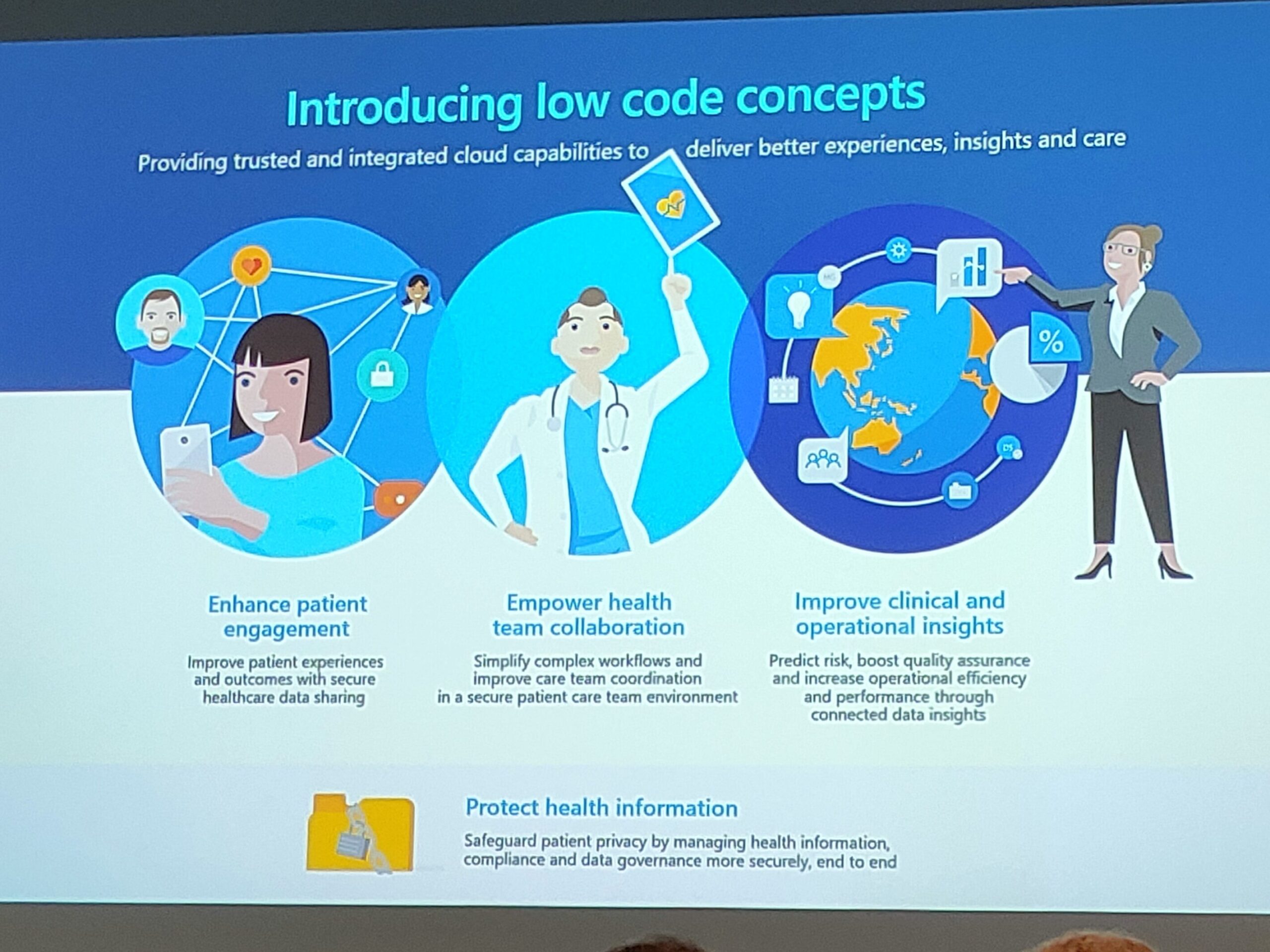
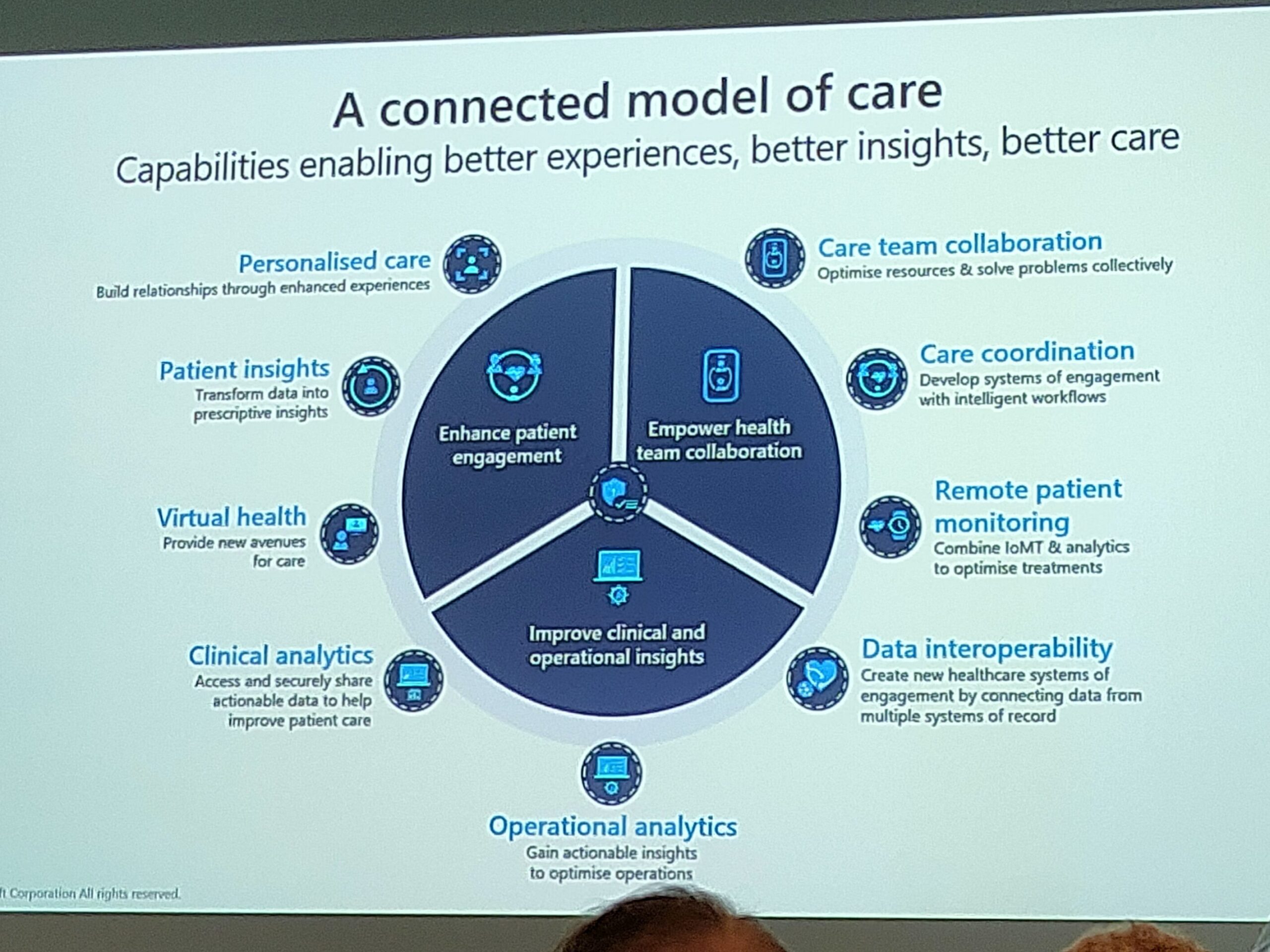
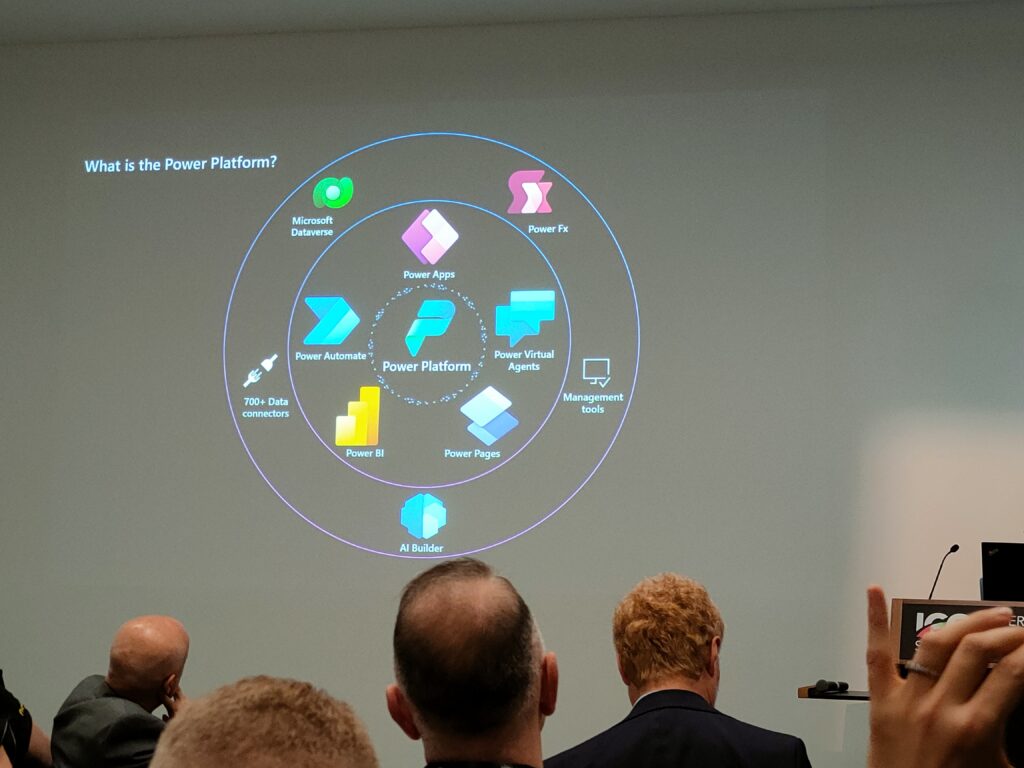
Low-code Development Masterclass
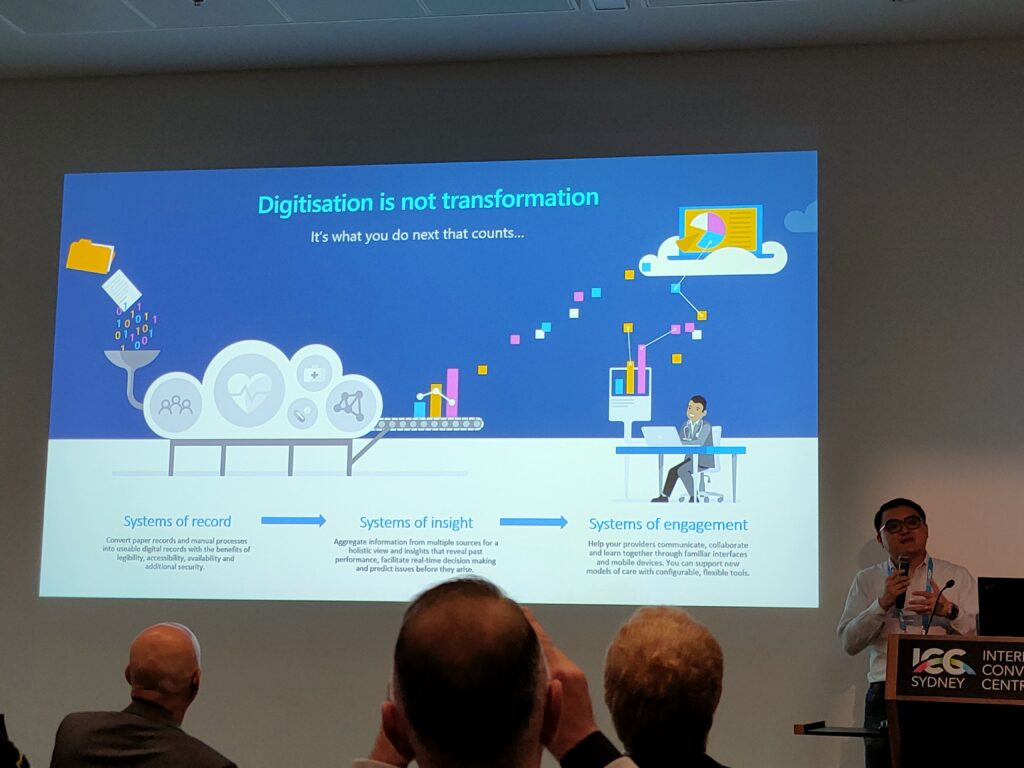
I was quite interested in seeing what this Masterclass was about. Led by Mr Jarrod Huang (Tech Lead Healthcare, Microsoft) and Mr Matt Pontel (Practice Lead – Modern Applications & Power Platform, Velrada), they showed a walkthrough of the Microsoft Power Platform and Power Apps to design a simple workflow process of booking an appointment for a patient through email. At the beginning of their presentation, they introduced the concept that “Digitization was not Transformation” (as what most companies equate to when talking about their digital transformation strategies), but it was what happened after the digitization process that counts. They argued that in order for enable a connected model of healthcare, “Systems of Record” (e.g. converting patient records and manual processes to EMRs and automated processes) should be integrated with “Systems of Insight” (e.g. providing holistic views and insights from multiple sources of data) and “Systems of Engagement” (e.g. digital systems that enable various stakeholders to communicate, collaborate and learn together) in the healthcare ecosystem, so that patients and clinicians could have better care insights and experiences. And this was where low-code concepts and applications could play a role – to enhance patient engagements, empower collaborations among the healthcare team and enhance both operational and clinical insights. Through there are many low-code applications that are available, the capabilities of Microsoft Power Apps seem to be quite impressive, especially when integrated with Microsoft Cloud. I will definitely be interested to see how these low-code platforms can help solve some of the issues that patients and clinicians in Singapore are facing.
The Digital Front Door to Enable Patient-centered Care
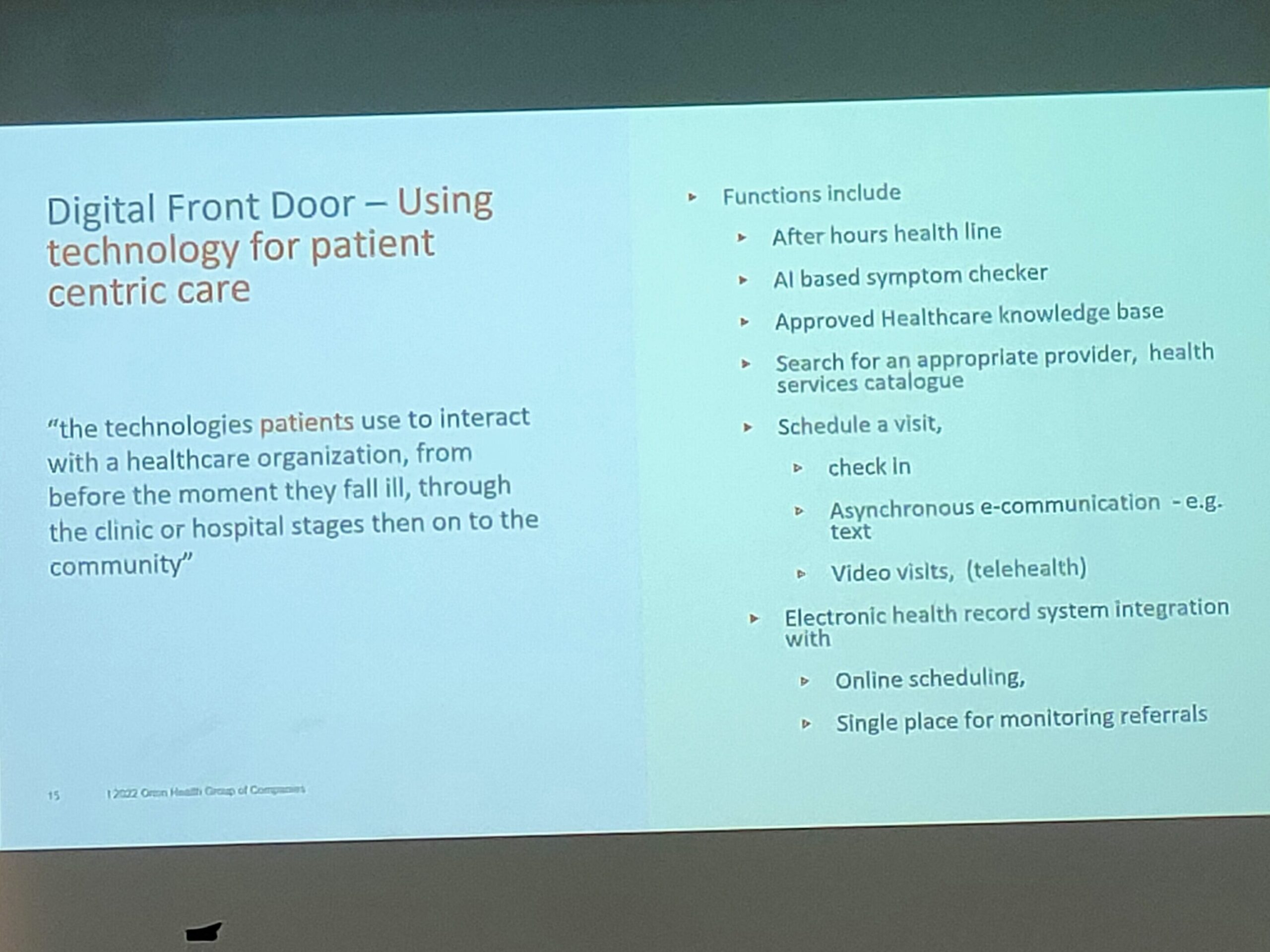
When I first heard the term “Digital Front Door“, it seemed to me just another hyped-up word for digital health technologies that facilitate the patients’ process of admission into hospitals or the emergency department. It was the first time I have come across this term, even though I have been keeping myself updated with the field. But according to the speaker Dr Chris Hobson (Chief Medical Officer, Orion Health, Ontario, Canada), this term actually referred to technologies that patients use to interact with a healthcare organization throughout their healthcare journey – from falling ill, all the way through their journey at the clinic or hospital, and after being discharged into the community. Examples of Digital Front Door systems include AI-based symptom checkers, healthcare databases, booking/scheduling systems, EMR/EHR systems, and after-hours health lines, etc.
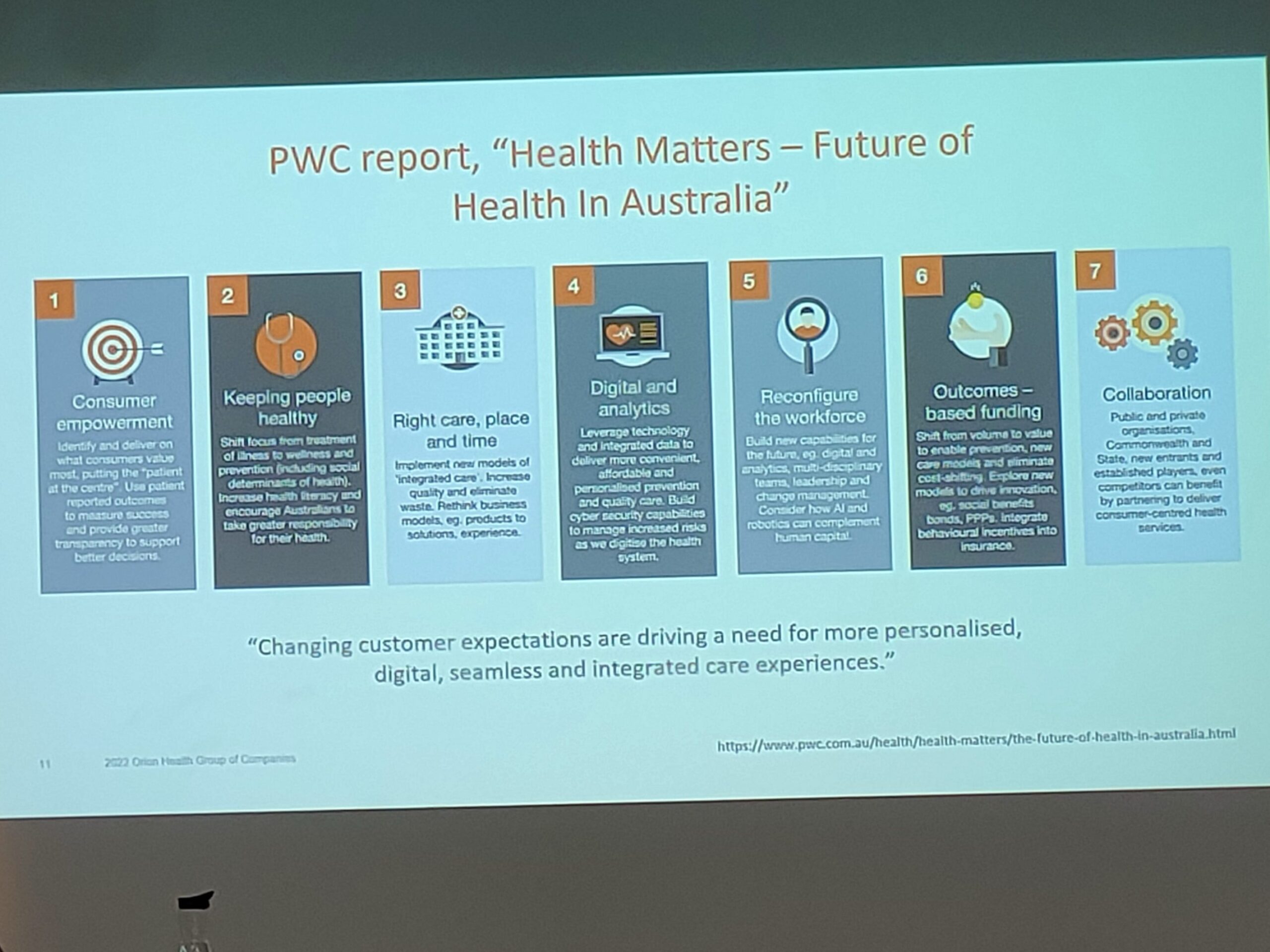
He quoted 7 focus areas from a PwC report that the Australian healthcare system needed to focus on in order to provide better patient-centered care:
- Consumer empowerment: In order for patients and consumers to take greater ownership of their healthcare, there is a need to increase access and transparency of health information and services in order to achieve better health outcomes. It is also important to build patient and consumer trust in public health institutions and the health ecosystem.
- Keeping people healthy: Increased health literacy is a way to drive desired health behaviors and improve health outcomes. Therefore, health promotion and prevention efforts are crucial. Furthermore, instead of depending on governmental efforts and public health institutions, initiatives should be focused on harnessing collective actions from individuals, carers/families, private sectors and industries to play a part and take ownership to change the community sentiment towards illness prevention.
- Right care, place and time: In order to better connect the healthcare ecosystem, there is a need to better define standards for health information exchange and health system interoperability, and leverage on virtual care technologies to connect remote communities and enable easier access to healthcare services at an affordable price. There is also a need to shift healthcare out of the hospital to the home, in a way that is commercially sustainable for all stakeholders involved.
- Digital and analytics: The concept of “Open Health” (open sharing of health information) should support digital health innovations, such as robotics and AI. Increased data access and data analytics can be used to shape healthcare investments, inform policy and regulatory decisions on healthcare and public health, as well as reduce healthcare costs. Of course, the issue of cybersecurity on health-related data is always important and as health information is increasingly being shared across various organizations, data protection, privacy, security and consents will becoming increasingly important for mitigating risks and building patient trust.
- Reconfigure the workforce: The healthcare workforce needs to evolve with the paradigm shift in the healthcare ecosystem. There is a need to collaborate to design alternative pathways to fast-track people who enter the healthcare workforce with skills in new technologies, changing mindsets and ways of working.
- Outcomes-based funding: A new framework for outcomes-based funding should be defined with broad consultation from various stakeholders, in order to support newer models of care that shift from “volume” to “value”. As part of defining this new framework, there is a need to identify alternative funding sources and mechanisms in order to create “value for money” for the patient/consumer, as well as support better affordability and sustainability across the public-private healthcare system.
- Collaboration: Last but not least, collaboration internally within the healthcare industry, as well as externally with other industries (e.g. technology, data analytics, infrastructure) will enable a more holistic healthcare system that is integrated for the patient and healthcare consumer.
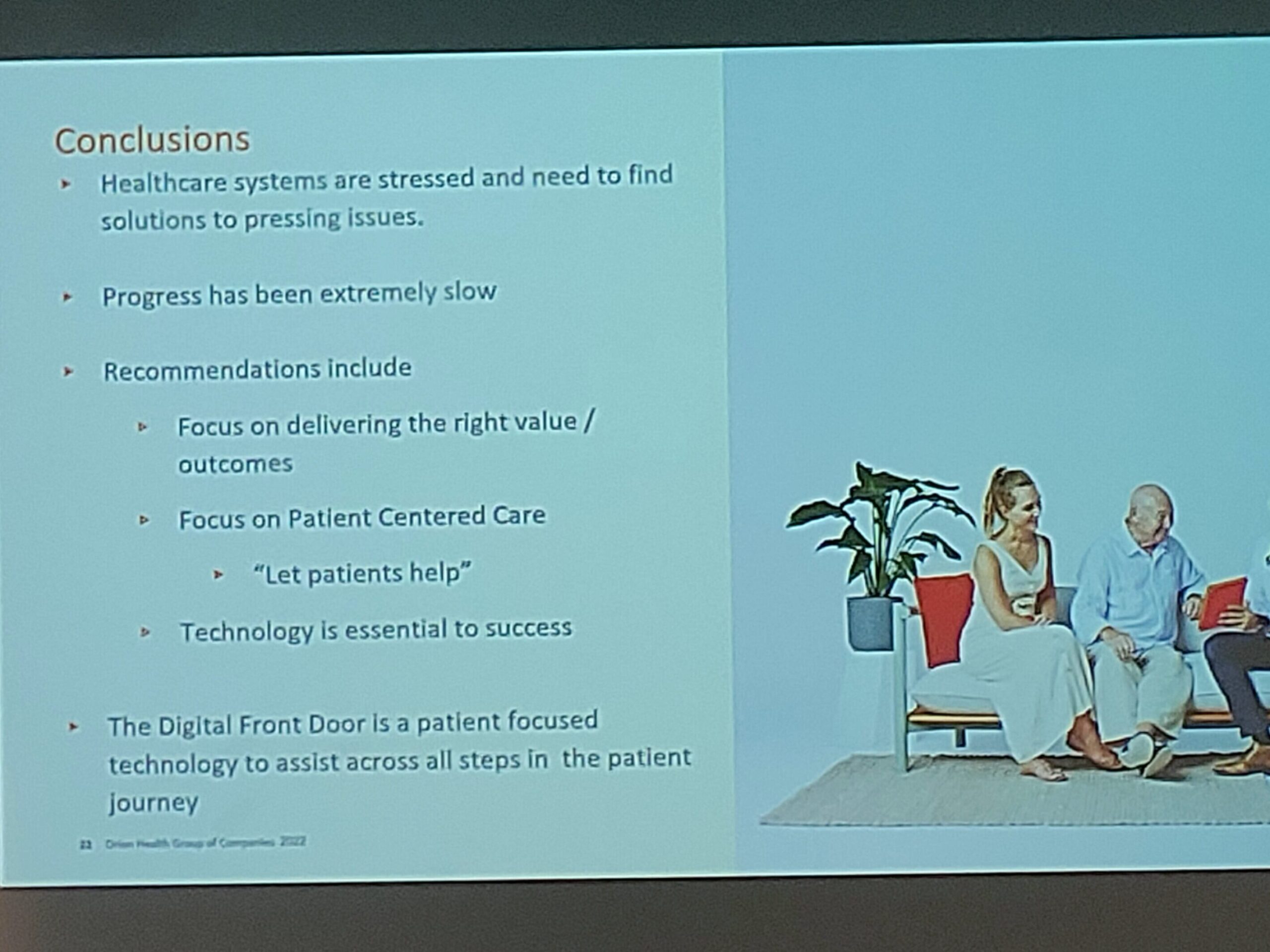
He concluded his talk by reiterating the importance of technology in improving healthcare systems and stressing the need to involve patients in their own care in order to obtain value-based outcomes.
Building Trust in Digital Health Apps
This panel session led by A/Prof Paul Cooper (Associate Professor of Health Informatics Management, Deakin University) was an interesting one. Together with his panel of experts (Ms Sonya Hilberts, International Health and Humanitarian Director of Programs; Dr Ben Bravery, Author of The Patient Doctor; Ms Nicole Liu, Founder of Kin Fertility; Ms India Hardy, Partner of PwC Australia; and Ms Karen Hay, Digital Transformation Lead Industry, Go-to-market Strategist, Public Sector, Salesforce), they discussed on a wide variety of issues on trust in digital health apps. The topics of discussion were wide-ranging – from the need to involve patients and clinicians in the designing journey of mobile health (mHealth) apps, to the need for a certification process for these apps, to information security and trust in governmental apps versus social media apps and Google, as well as AI-driven systems and whether mHealth apps for therapeutic purposes should be regulated by the authorities. All-in-all, it was a very interesting panel session with several ideas that were thrown about. Hopefully, some of the ideas would become reality with time.

Getting SMART with FHIR Workshop
One of the technologies that I realized has been picking up quite fast is FHIR (Fast Healthcare Interoperability Resources, pronounced as “fire”) – a Health Level Seven International (HL7) standard for applications and data formats for health information exchanges. There are 5 levels according to the FHIR website:
- Level 1: Basic framework on which the specification is built
- Level 2: Supporting implementation and binding to external specifications
- Level 3: Linking to real world concepts in the healthcare system
- Level 4: Record-keeping and data exchange for the healthcare process
- Level 5: Providing the ability to reason about the healthcare process
There are many applications that have leveraged on the FHIR specifications. A non-exhaustive application list was provided in the workshop.
- SUKI: AI dictation assistant
- Juxly: EMR patient management system
- RIMIDI: Cardiometabolic DM platform
- EMORY Healthcare: DBS Caretrek app
There were also 2 publications that were mentioned in the workshop:
- AAFP Innovation Labs Report: An AI Assistant Reduces Documentation Burden – Evaluating the Suki Assistant
- Health Informatics on FHIR: How HL7’s API is Transforming Healthcare (2nd Ed)
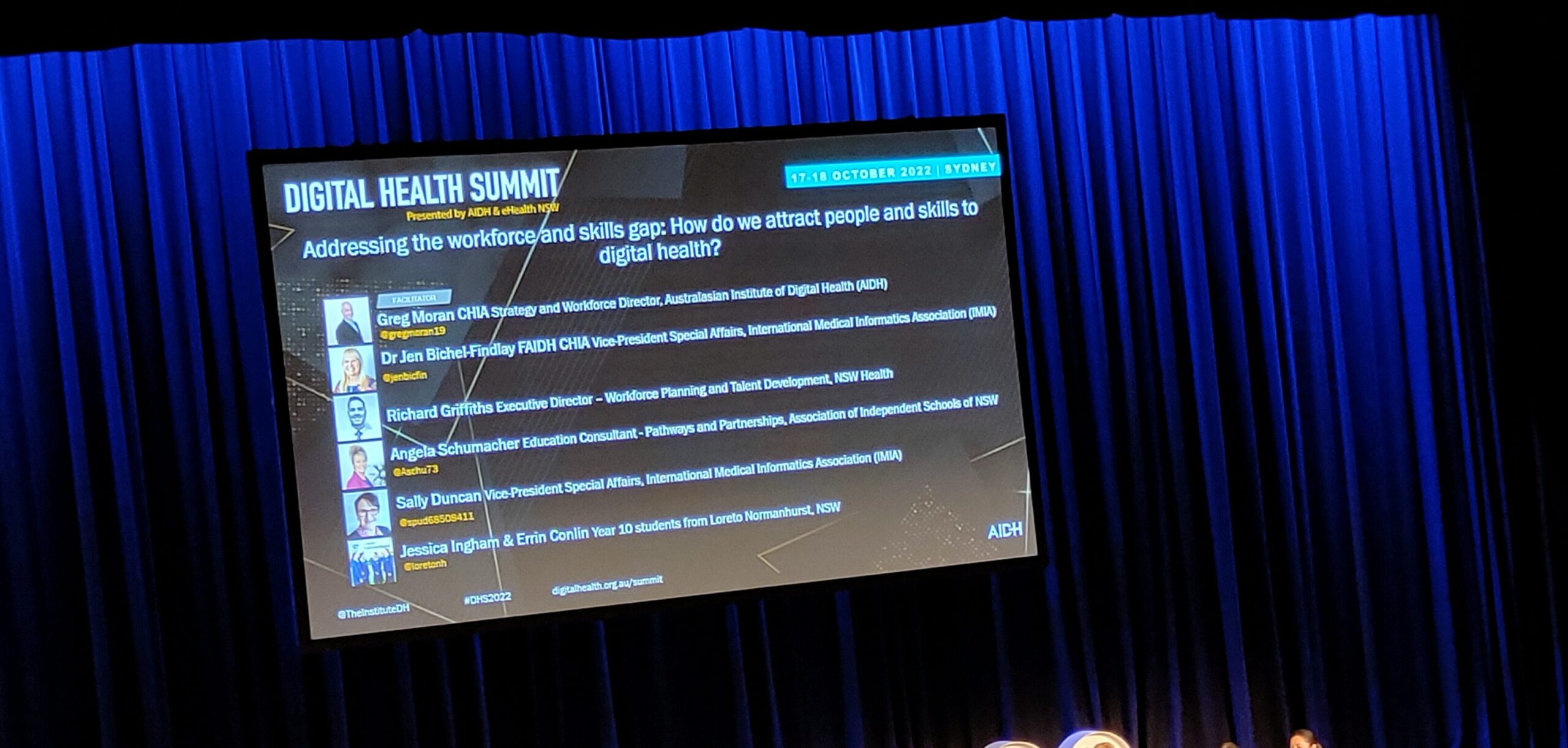
Redefining the Digital Health Workforce to Address the Workforce and Skills Gap
While there were several sessions throughout the conference, what really struck me were the sessions on how to attract people with the relevant digital health skills to address the workforce and skills gap. Ms Angela Schumacher (Education Consultant, Association of Independent Schools of NSW) gave a wonderful talk on how she partnered with schools to provide students with opportunities to work on digital health projects that aimed to solve real-life healthcare issues. During the panel session, there were also 2 students who were invited to talk about their experiences with their digital health internship projects. They were really interested in their projects and the opportunities opened their eyes to the world beyond healthcare – one that was not just about medicine and clinical practices, but to domains like user-centered designs, human-computer interactions and even the medical humanities. The takeaway for me was that there were various digital health workforce initiatives that the Singapore healthcare sector could consider in terms of partnering with schools besides traditional curriculum development, work experience and internships, including digital health ambassadors, educating teachers (not just students), incubator programs, design challenges, hackathons and training academies, etc.


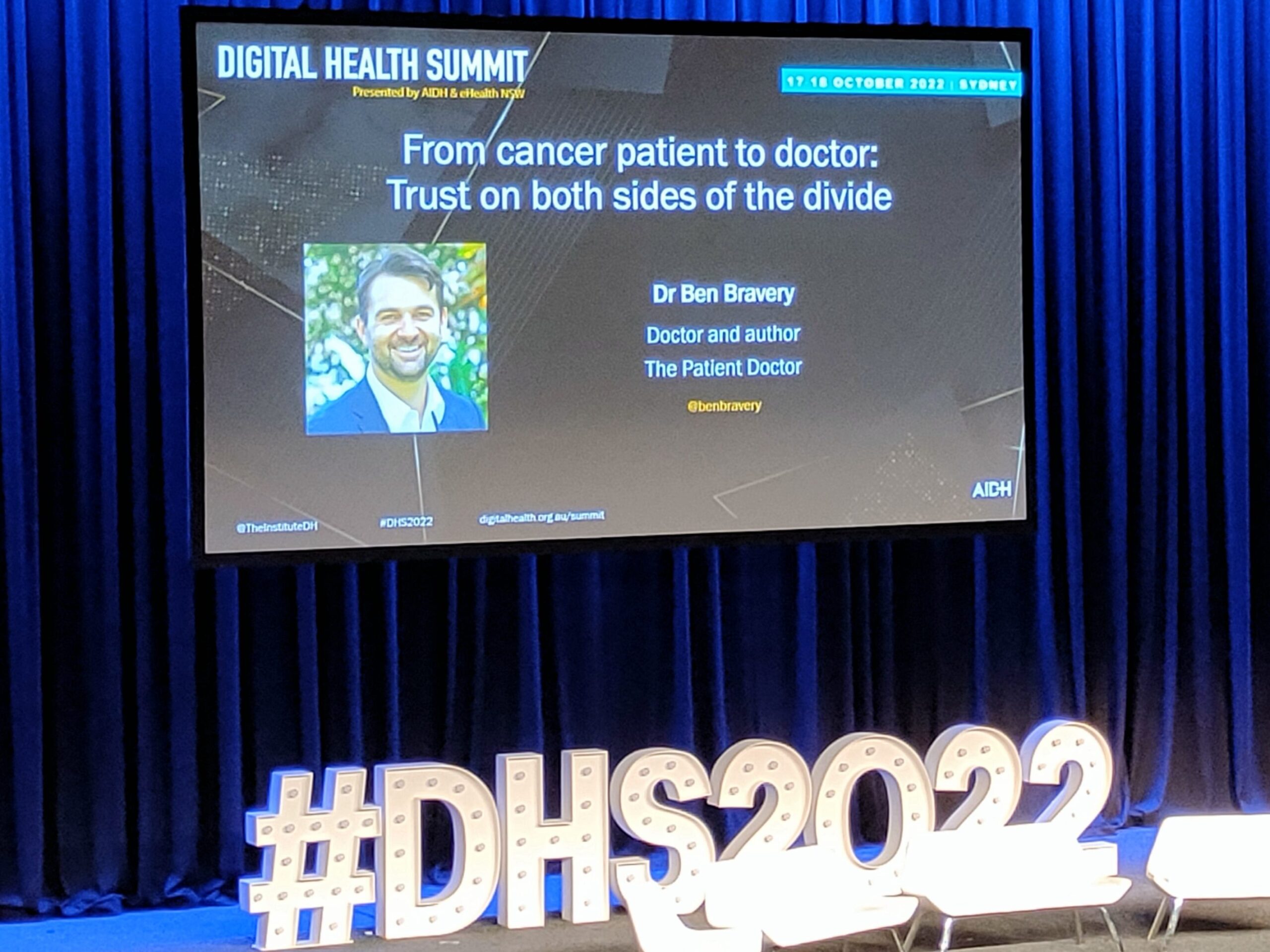
“Don’t Only Teach What Illness Is, Teach What It Feels Like” – The Patient Doctor
Perhaps the most striking part of the conference for me was the session by Dr Ben Bravery – the author of the memoir The Patient Doctor. Unlike the traditional doctors who went through medical school, he was actually a zoologist and science communicator who was diagnosed with colorectal cancer at the age of 28. After going through the experiences of cancer therapy and the healthcare system from the patient’s end, he decided to have a career change and became a doctor in 2018, and is now undergoing training in psychiatry. Having experienced both ends of the spectrum as a patient with a chronic disease and training as a medical student, resident and doctor, he is now a strong advocate on training medical and healthcare students not just head knowledge and practice from the practitioner’s point-of-view, but more importantly, from the patient’s lens – which he believes will truly bring about patient-centered care by putting the patient at the center of the care journey. His anecdotes were not only entertaining, but also reflected his passion for patients – which I thought was truly different and inspiring from other doctors and healthcare professionals whom I have come across. He has inspired me to buy his book “The Patient Doctor” to read about his experiences, which I will write about another time.
Presentation: Metaverse for Digital Health Education
Of course, I also did a presentation at the conference. I believe mine was the only presentation in the Digital Health Summit that focused on the Metaverse for Education (“Eduverse”).
As we know, COVID-19 has forced many educational programs to adopt online and/or hybrid practices. Technologies that have been used to improve learner experience include video recordings, learning management systems, and more recently, Zoom, virtual/augmented reality (VR/AR) and serious games. However, these practices still have their own limitations, such as providing immersive, collaborative and engaging social learning experiences, particularly among the Millennial and Gen Z generations of learners. We developed a in-house metaverse gallery where participants could join as avatars and explore the gallery as part of a synchronous tour or asynchronously in their own time. Being the future of the internet, the metaverse is envisioned to support multiple technologies, including augmented/virtual reality, AI and advanced connectivity to link the physical and digital worlds. Its role in digital health education can potentially be a game-changer to learner experience and pedagogical practices.
The learning objectives of my presentation were to:
- Introduce the concept of the metaverse and its application potential in healthcare; and
- Identify user perceptions and experiences of using the metaverse for digital health education.
Summary
The Digital Health Summit was an interesting and eye-opening experience as to how Australia is transforming to embrace digital health technologies. The talks and panel discussions showed that besides learning about digital health innovations, there is a need to change education norms and clinical practice culture, as well as remember that amidst all these innovations, the center of it all is still the patient.
I certainly hope that next year’s MedInfo23 will provide a broader and more international view on digital health across the world!