In recent months, there have been several system failures with the health IT systems in public health institutions in Singapore. According to local news, the system outages were due to failure in hardware devices in data centers. During a time when hospitals are overwhelmed with extra workloads from the COVID-19 pandemic, these failures put on additional pressure on the healthcare system, as well as on healthcare professionals.
According to reports, downtime procedures had to be activated at the affected institutions, which included some operations being run using alternative systems or through manual documentation. Many patients had their appointments delayed or rescheduled due to the incidents, and waiting times at the affected institutions were also delayed by up to an hour. The dispensing of medications was also delayed.
Electronic medical record (EMR) systems
One of the upcoming systems in the healthcare sector in Singapore is the Epic EMR (electronic medical record) application (also known as ‘Epic‘) by Epic Systems Corporation. The parent company is a private American company in the health informatics industry and it is one of the major electronic medical record (EMR) system providers for US hospitals, with other international offices in places like the UK, Netherlands, Dubai, Australia, Singapore, Norway and Denmark, among others. Epic is a proprietary EMR software with a database management system that supports functions related to patient care, such as clinical systems for doctors, nurses and other care providers, registration and scheduling systems, lab systems, pharmacy systems and billing systems for insurers. Epic is used by many of the top-ranked hospitals and medical schools in the US, including the Cleveland Clinic, Cedars-Sinai Medical Center, Johns Hopkins Hospital, Mayo Clinic and the University of California (UC) Davis Medical Center.
Unfortunately, while Epic had worked well in the US, there were many criticisms about its application being deployed in other countries. For example, the experience in Denmark hospitals ranged from being frustrating to disastrous. The design of Epic was so entrenched in the US healthcare system and culture that there wasn’t enough flexibility to cater it towards the Danish healthcare IT systems, health insurance systems and medical culture. Some issues that surfaced included the fact that the medical terms in Epic were not tagged for easy translation to the Danish healthcare system. In addition, Epic had difficulty integrating with the national medical record system in Denmark. In short, the system was “clunky” and “chunky” to the healthcare system, leading to frustration among both healthcare professionals and technical specialists. In the UK, the Addenbrooke’s Hospital and General Practitioners (GPs) in The Cambridge University Hospitals NHS Foundation Trust also experienced serious problems after their installation of Epic. According to reports, the system became unstable, resulting in the rerouting of ambulances to other hospitals and also issues with their blood transfusion and pathology services.
Validation of EMR systems
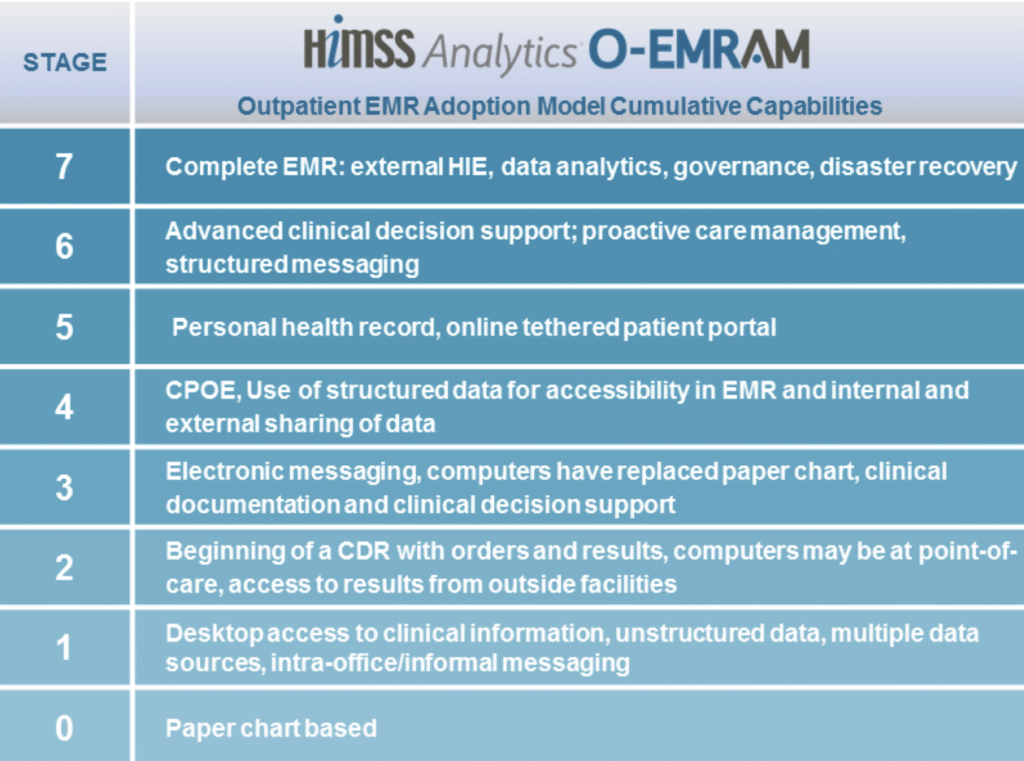
With the advent of COVID-19, many hospitals locally and globally are finding ways to improve their EMR systems. For example, in November 2020, Singapore’s Ng Teng Fong General Hospital (NTFGH), which is a 700-bed hospital under one of the three healthcare clusters in Singapore – the National University Health System (NUHS) cluster – underwent a successful revalidation of their Epic EMR system. Needless to say, such (re)validations are important as there may be significant impacts on workflow processes, clinical care and patient safety. Their revalidation process involved Stage 7 of the Electronic Medical Record Adoption Model (EMRAM) by the Healthcare Information and Management Systems Society (HIMSS), which evaluated 4 aspects on how their EMR system could:
- Improve patient safety by providing clinician access to critical information as and when needed;
- Increase patient satisfaction through reducing time and errors in care delivery and providing the right information at the right time for both clinicians and patients;
- Support clinicians by ensuring that the content in the system and workflow could meet the clinical needs of the hospital, yet maintaining compliance with approved standards; and
- Provide data security through appropriate level of access and use of the EMR data by clinicians and other hospital staff.
Should healthcare providers rethink their digital healthcare strategies?
Amidst the plethora of digital health technologies that have entered the market since COVID-19 (such as mobile health apps, health-related websites, patient portals and other devices), the market research firm Frost & Sullivan advocates that healthcare providers should indeed rethink their digital healthcare strategies. The company argues that having digital health technologies are no longer a utility, but a growth or survival case. If one does not rethink their digital healthcare strategies, they may be lagging behind their competitors, which may lead to negative consequences for the company/organization.
One of the common approaches to leverage on digital healthcare technologies by healthcare providers is the use of platforms to consolidate various applications into a “one-stop shop”. Another approach is the use of health data to personalize the patient experience towards call-to-actions. EMRs were not originally designed to be patient-facing tools. But with non-traditional players getting into the market, the competition for a well-designed healthcare platform with integrated solutions that can provide personalized action-oriented information to clinicians and patients in a more convenient matter, is more stiff than ever before. For example, Amazon has been coming up with a variety of digital health initiatives ranging from its PillPack digital pharmacy to catering Alexa’s digital voice assistant features for healthcare and getting into the wearable space. Apple has also enhanced its efforts to improve its Apple Watch features. Healthcare Triangle – a healthcare IT company focusing on cloud solutions and data analytics – has recently launched a local Singapore branch with the aim to help healthcare companies in the Asia-Pacific scale up their digital solutions through their cloud-based platforms. Even health insurance companies are starting to leverage on technologies such as cloud computing, robotic process automations, mobile apps, chatbots and voice-assistants, and virtual/augmented reality, to provide better and more personalized services to customers.

Digitally transforming healthcare is “more than meets the eye”…
As the search for a more integrated solution continues, one must remember that navigating healthcare is fundamentally complex. Having a “one-stop shop” is just the beginning. The last two years of the COVID-19 pandemic has taught us that going digital is not only inevitable, but is the way to go in the new normal. However, the goal of ultimately providing a truly seamless patient care journey is still far away as the world grapples with the wide variety of medical problems and clinical practices, different healthcare settings and healthcare systems, different health insurance schemes, different regulatory considerations and data privacy and cybersecurity concerns, among others. We should celebrate the quick wins of digital health transformation as these “low-hanging fruits” bring us one step closer to our goal. As Neil Armstrong once said, “That’s one small step for a man, one giant leap for mankind.“

