The MedInfo23 conference was a very inspiring conference, where I got to learn many different practices and innovations from institutions and organizations all over the world. Besides the keynote sessions at the beginning and end of the day, there were also many different parallel sessions that were very interesting and engaging – ranging from topics in the domains of health data sciences and artificial intelligence (AI), global health informatics, standards and interoperability of technologies, and data-enabled and social care; to new frontiers for learning, human/organizational and social aspects, innovating for quality outcomes, and workforce development and leadership in digital professionalism. In terms of abstracts submissions (which were in fact paper submissions), there were 662 submissions from 53 countries from all the International Medical Informatics Association (IMIA) regions. In the end, the final program incorporated 281 papers (237 full papers, 44 student papers), 139 posters and 83 panels, tutorials and workshops – this showed how large-scaled this conference was!

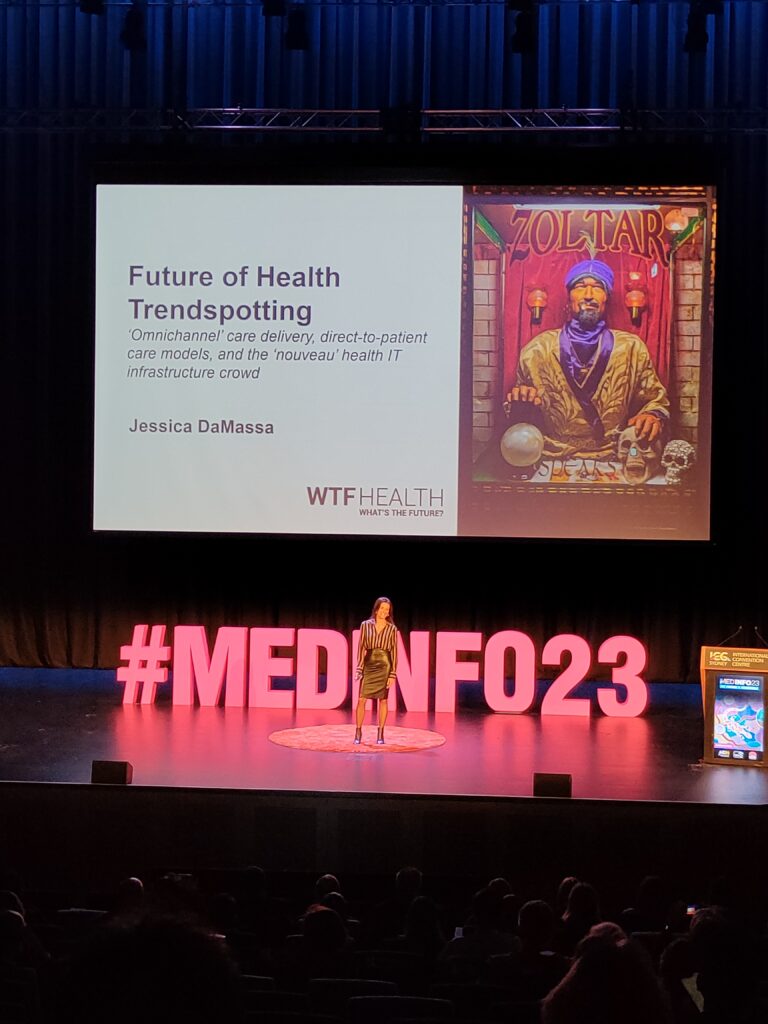
In this post, I will focus on digital health trends that caught both my eye and attention. The speakers of these trends were internationally known individuals – the first was Ms Jessica DaMassa, the creator of WTF Health (What’s The Future?) – an ‘IT girl” of health tech interviewing, who conducted over 100’s of interviewers with the ‘Who’s Who” of health tech innovation, ranging from health tech startups, venture capitalist investors, innovators, pharma companies, hospital systems, etc, in order to spot the latest trends and what’s next in the future of health tech innovations. In her talk, she spoke about how the digital health strategies and spending of organizations changed during COVID-19 (2020-2021) to focus on telehealth, to innovations that provided the ‘digital front door’ for patients/consumers (2021-2022, i.e. innovations that used virtual as a way to get into the health system). Her prediction for innovations in the post-COVID era (2022-2023 onwards) was what is termed as “omnichannel” innovations – health tech that uses virtual as its own place in the health system. The aim of these omnichannel innovations is to provide direct-to-patient care models that will enhance the health experience of the future that modern consumers expect of their care. Already, many large companies, such as CVS Pharmacy, Walgreens and Amazon have embarked on this model, by providing a one-stop shop that contains a combination of telehealth services, online pharmacy services, as well as in-home care. The paradigm shift of healthcare towards patient-centric care implies that many healthcare companies/organizations will have the following characteristics moving forward into the future:
- No/limited brick-and-mortar footprints;
- Telehealth-based services;
- Flexible staffing;
- Incorporating technologies that streamline operations, triaging and fulfillment;
- Having direct relationships with drug manufacturers;
- No need to contract with payers; and
- Catering for a national market.
Another talk that I was very impressed by was the one by OpenNotes – an international movement focused on making healthcare more transparent and open by encouraging clinicians to share their clinical SOAP notes. I am not able to repeat the amazing presentation given by Liz Salmi, the Founder of OpenNotes, but I was fortunate enough to find an interview with her by WTF Health!
Another paradigm shift that was described was in terms of the health information technology (IT) system of the future. While we are all familiar with the large health IT organizations in this space right now, such as Epic, Oracle, Cerner and MediTech, the trend of health IT companies is going to be based on 4 types:
- “Layer on Top” companies: These are companies that provide platforms that integrate various services (e.g. telehealth, remote monitoring, care coordination, AI-enabled conversations, data analytics, etc) to provide a more seamless patient journey experience (e.g. StoryHealth, Artera, HealthSnap, KeyCare).
- “Move and Analyze Data” companies: Using applied analytics, AI expertise and automated solutions, these companies leverage on the large amounts of healthcare data from the various health IT platforms to provide actionable insights to patient care, yet maintaining the privacy and security of the data (e.g. Health Gorilla, Ribbon Health, Turquoise Health, LexisNexis).
- “DIY EMR” companies: These companies provide technology-driven shared health data platforms that enhance the interoperability of electronic medical and health records with various healthcare services and third-party payers and purchasers, so that both the healthcare professionals’ and patients’ experience are cohesive and holistic (e.g Privia Health, Zus Health, 98point6).
- “And Both” companies: These companies offer insight into the patient’s health holistically by combining clinical (e.g. health parameters) and non-clinical data (e.g. demographics, environmental, financial) in a customer relationship management platform, through the linkage of a whole suite of products and capabilities, including AI, virtual care, data platforms, a patient care coordination portal, and a commercial portal, so that actionable programs and follow-up care can be personalized to the patient (e.g. Salesforce Customer 360)
As you can see from these new and upcoming digital health models, there is going to be a paradigm shift in terms of the health ecosystem at scale, internationally, and we, as healthcare professionals and healthcare providers, must learn to embrace these innovations and open platforms, in order to keep up with the speed of innovation that is happening worldwide.
Domains That Caught My Attention
There were 4 broad domains that came close to my heart in this conference.
(1) The Power of Co-design
The first was about the Power of Co-design – the importance and lessons learnt about the co-design of innovations from an international perspective. While many healthcare professionals are interested in innovations, both for education and for patient care, there are very few of us who actually undergo the co-design process to make the tech innovation more human-centered. Co-design is a process that involves multiple stakeholders (including healthcare professionals, patients, administrators, educators, students, and any intended target user group) in the design and development of products, services or systems. These stakeholders are usually actively involved in the envisioning and creation process of a potential solution to meet an unmet healthcare gap. The goal of co-design is to create innovations and solutions that are more relevant, effective and satisfying to users. By nature, co-design is a collaborative process and is participatory in nature. The benefits of the co-design approach are:
- It creates solutions that are more useful and user-centered;
- It leads to a better understanding of user needs;
- It increases user engagement and collaboration; and
- It helps in stakeholder alignment and buy-in.
The co-designing process can be time-consuming and resource-intensive, especially when the healthcare problem is a big one to tackle. However, my takeaways are as follows:
- Co-design takes time: A good co-designing process requires regular meet ups for planning, delivery, organization, etc. Time must be allocated for by all who are involved in the co-designing process.
- Recognize small amounts of co-design: The solution will usually take a long time to complete. As such, any small steps that are small “wins” should be recognized (and maybe celebrated) to keep the morale and motivation of the team up.
- Power of co-design leads and completing the co-design cycle: The people leading the co-design process should be cognizant of the co-design process to guide the others, especially stakeholders, in the correct direction. These leads should also be involved throughout the whole co-design process in order to maintain continuity.
- Transparency is key: There is a need for transparency to the stakeholders involved in the co-design process on how much time and effort (potentially logistics and/or payments) is needed from/ provided to them so that they are fully prepared to take this process on.
- Communication takes time, but is imperative: There is a need to ensure that proper communication occurs throughout the co-design process among the team members and stakeholders, so that everyone is on the same page and agrees to the changes made to the solution. There will be times when the ideal solution may not always be feasible/practical, and the potential for conflicting opinions can also make the decision-making process more complex.
- Know your audience: This forms the basis of the whole co-designing process, as the target audience is the one who is going to use the innovation/solution. Therefore, the team must always keep in mind who they are co-designing for, and continuously put themselves in the shoes of the user.
(2) Developing Capability in AI for Healthcare
The 2nd domain was in Developing Capability in AI for Healthcare. As we all know, AI represents a significant opportunity for the healthcare sector to drive better patient and business outcomes, while capitalizing on its new growth potential. According to Accenture’s analysis of AI in Healthcare, the top ten AI applications in health are:
- Robot-assisted surgery,
- Virtual nursing assistants,
- Administrative workflow assistance,
- Fraud detection,
- Dosage error reduction,
- Connected machines,
- Clinical trial participant identifier,
- Preliminary diagnosis,
- Automated image diagnosis, and
- Cybersecurity.
These key clinical AI applications can potentially create a US$150 billion in annual savings for the US healthcare economy by 2026. The advent of AI in healthcare not only implies that the future of the healthcare workforce is dependent on AI, but also suggests that there will be changing roles for healthcare workers in time to come. Figure 1 shows the changing roles of healthcare workers as AI becomes more prevalent in our daily work.
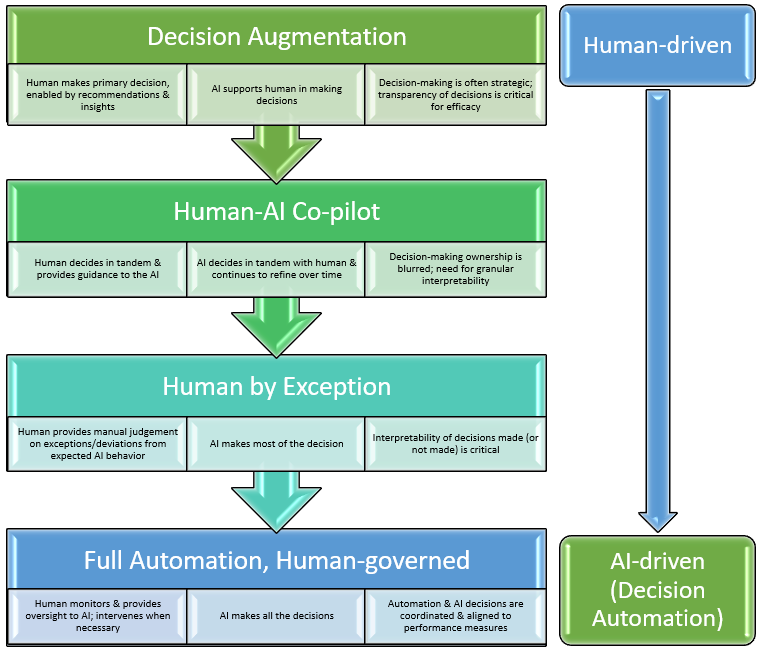
The NHS AI and Digital Healthcare Technologies Capability Framework has defined 5 archetypes that describe healthcare workers working at the interface of AI and digital health. The workforce archetypes are:
- Shapers: They set the direction for AI policy and governance at a national level;
- Drivers: They are the leads and champions of AI development and deployment at a regional/local level;
- Creators: They create AI technologies for use in healthcare settings;
- Embedders: They implement, evaluate and monitor AI technologies that are deployed in healthcare; and
- Users: They use AI technologies in their healthcare environments.
Each archetype has different knowledge and skills required to develop, implement and/or use AI and digital healthcare technologies – therefore, they each need a different and specific set of educational needs. Although most healthcare workers have responsibilities associated with one of the archetypes, they are not mutually exclusive and may exist in different combinations when the healthcare professional is involved in multiple projects.
In order to build a digital workforce capability at scale, there is a need to embed certain elements of the capability framework in AI and digital health education and training. These include:
- Showing that digital can work;
- Developing new career structures;
- Embedding digital early in training;
- Supporting existing workforce through continuing education; and
- Enabling decision-making by people who understand digital and AI.
For healthcare professionals who are already working in their clinical setting, the most practical way would be to support them through continuing education. The methods of engagement can include online learning, self-led reading materials, case studies, as well as project-based learning – of which the latter caught my attention due to its ability to provide practical and applied learning.
(3) Establishing a Digital Health Validitron
The 3rd domain was in the establishment and implementation of a Digital Health Validitron, as exemplified by the Centre for Digital Transformation of Health at the University of Melbourne. This is a research platform that not only supports the development of digital health innovations, but also focuses on the implementability, workflow integration and evidence generation in clinical practices. This requires 3 components that work hand-in-hand in order to bring a digital health idea into production, implementation, and validation: (i) methods expertise, (ii) a simulation lab for co-designing and prototyping, and (iii) a sandbox for testing and demonstration (Figure 2). This powerful combination can definitely help in bringing the ideas of our healthcare professionals to fruition!

(4) Developing a Confident Digital Health Workforce
The Australian Digital Health Agency has developed a National Digital Health Workforce and Education Roadmap that has been endorsed by the Australian Government to improve the digital capabilities of the healthcare workforce – which is defined as:
“A workforce confidently using digital health technologies to deliver health and care will be required to address the technology adoption challenge… and embrace the changes and opportunities created by digital health innovation.”
By the Australian Digital Health Agency
Their report describes 8 digital role profiles to help healthcare organizations understand the different requirements of the healthcare workforce as these organizations continue to undergo digital transformation. These digital profiles include:
- Patient, consumer and carer;
- Frontline clinical;
- Digital champion;
- Clinical and technology bridging;
- Technologist;
- Leadership and executive;
- Business, administration and clinical support; and
- Education and research.
More details can be obtained from their forward-looking report. These profiles may be useful to consider when healthcare organizations are intending to improve the digital literacy of their staff.
Our Presentations at MedInfo23
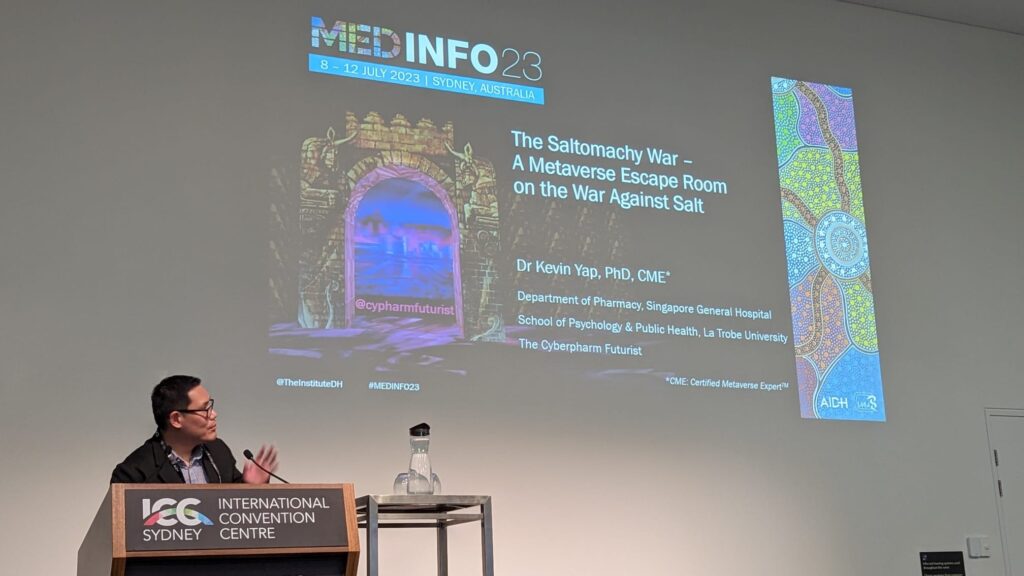
I also had the privilege of presenting some of our work at the MedInfo23 conference, together with my friends and collaborators. More details can be accessed at:
| Yap KY. (11 Jul 2023) Developing a digital health Metacademy for continuing professional education. Paper presented as poster presentation (Paper 17) at MedInfo23 – The 19th World Congress on Medical and Health Informatics, International Convention Center (ICC) Sydney, Sydney, Australia. Organized by the Australasian Institute of Digital Health (AIDH) and the International Medical Informatics Association (IMIA). |
| Yap KY, Liem M. (8 Jul 2023) How to create good stories for serious games in healthcare: Deconstructing storytelling through Squid Game. Paper presented as a 40-minute main conference academic workshop (Paper 15, Session 12: Human, organisational and social aspects, Room C4.1) at MedInfo23 – The 19th World Congress on Medical and Health Informatics, International Convention Center (ICC) Sydney, Sydney, Australia. Organized by the Australasian Institute of Digital Health (AIDH) and the International Medical Informatics Association (IMIA). |
| Bin Ahmad A, Tan S, Yap KY. (9 Jul 2023) The Saltomachy War – A metaverse escape room on the War Against Salt. Paper presented as oral presentation (Paper 32, Session 61: Human, organisational and social aspects, Room C4.6) at MedInfo23 – The 19th World Congress on Medical and Health Informatics, International Convention Center (ICC) Sydney, Sydney, Australia. Organized by the Australasian Institute of Digital Health (AIDH) and the International Medical Informatics Association (IMIA). |
| Goh A, Budijono B, Lim C, Chew EH, Yap KY. (10 Jul 2023) An in-house developed probiotics database e-reference information for healthcare professionals. Paper presented as oral presentation (Paper 327, Session 79: Information and knowledge management, Room C4.1) at MedInfo23 – The 19th World Congress on Medical and Health Informatics, International Convention Center (ICC) Sydney, Sydney, Australia. Organized by the Australasian Institute of Digital Health (AIDH) and the International Medical Informatics Association (IMIA). |
References
- DaMassa J. WTF Health. Available at: https://www.wtf.health/. Accessed 21 Aug 2023.
- Christiansen P. Artificial intelligence: Healthcare’s new nervous system. Accenture Insight Driven Health Report. 30 Jul 2020. Available at: https://www.accenture.com/au-en/insights/health/artificial-intelligence-healthcare. Accessed 21 Aug 2023.
- NHS Health Education England. Executive summary: Developing healthcare workers’ confidence in artificial intelligence (AI) (Part 2). Available at: https://digital-transformation.hee.nhs.uk/building-a-digital-workforce/dart-ed/horizon-scanning/developing-healthcare-workers-confidence-in-ai/executive-summary. Accessed 21 Aug 2023.
- Centre for Digital Transformation in Health. The Digital Health Validitron. University of Melbourne. Available at: https://mdhs.unimelb.edu.au/digitalhealth/our-work/validitron. Accessed 21 Aug 2023.
- Australian Digital Health Agency, 2020 Sep. National Digital Health Workforce and Education Roadmap. 1st Edition. Australian Government: Sydney, NSW. Available at: https://www.digitalhealth.gov.au/sites/default/files/2020-11/Workforce_and_Education-Roadmap.pdf. Accessed 21 Aug 2023.