Two recently published landmark RCTs in NEJM AI finally show the evidence on AI scribes as productivity tools and whether it reduces clinician burnout.
Since the hype of AI scribes, there has been a mix of both excitement and skepticism in the healthcare world. Various companies have sprung up claiming that ambient AI scribes can dramatically reduce clinician burden and enhance productivity in hospitals. Every vendor claims that AI scribes can free up documentation and create more time for patient care. But is this really true? Finally, two published randomized clinical trials (RCTs) have debunked the claims of this hype.
How Do AI Scribes Work?
In short, AI scribes use speech recognition, natural language processing and other machine learning methods, including Generative AI (Gen AI) to automatically transcribe clinician-patient conversations during consultations into medical notes. Some scribes that are integrated with hospital/healthcare systems can also convert the conversations into structured clinical notes be stored and archived in electronic medical records. Since these tools can automate tasks like transcribing and charting, there have been many claims that these scribes can reduce administrative burden and improve patient engagement. This YouTube video by Canada Health Infoway neatly summarizes the purpose and use of AI scribes.
Players in the AI Scribe Space
There are many AI scribes today. Some of the more popular ones out there include, but are not limited to:
- DeepScribe – This was one of the first AI scribes that I had come across in my readings, which intrigued me. Last year, the company collaborated with CardioOne – a cardiology care platform – to provide their scribe technology to cardiology clinicians. Recently, the company has recently partnered with Flatiron Health to integrate and optimize their tool in OncoEMR (their cloud-based electronic medical records for oncology).
- Notable Health’s Sidekick – Notable’s AI scribe was another one that I came across early on. Since its inception, it has enhanced its features with their built-in co-pilot (Sidekick), and a low-code builder with Flow AI, which enables automated understanding of workflows through conversations, real-time logic understanding, pattern recognition and intelligent suggestions.
- Microsoft DAX Copilot – Begun as part of a 120-day AI Tech Sprint competition in 2024, DAX Copilot seems to be one of better-known scribes around and is used by more than 20,000 clinicians across the US Department of Veteran Affairs (VA) network and more than 600,000 users worldwide. Built on Microsoft Azure and based on a responsible AI framework, this copilot can also integrate with the EPIC electronic health record (EHR) system for a more seamless scribing of clinical notes.
- Nabla Copilot – Nabla was one of the early adopters of GPT-3 when it was first released in 2020. Focused on speed and simplicity, Nabla was born out of Paris as a Chrome extension-based AI digital assistant for doctors, but is now enhanced to be available as a mobile app, and also connects to a variety of EHRs through a plug-and-play module.
- Abridge AI Scribe – Coming from another healthtech startup that gained lots of traction in the US, this scribe was developed by a cardiologist before OpenAI and LLMs were mainstream. Described as being “life-changing”, “magical”, and “one of the most important paradigm shifts” by clinicians and hospital executives, the app now supports 14 foreign languages, including Haitian Creole, Brazilian Portuguese and Punjabi, among others.
- Amazon HealthScribe – Amazon Web Services (AWS) has also entered into the ambient AI scribe market with a HIPAA-eligible service to streamline the documentation of clinical consultations. Powered by Amazon Bedrock, its Gen AI platform, HealthScribe not only provides a cohesive summary of the conversation, but it also segment the conversations into categories based on the relevance and context
- Suki Assistant – Headquartered in San Francisco, the company says that their AI Assistant does more than just a scribe – it is actually a virtual digital assistant available as an iOS app, as well as integrated with EPIC EHRs! In fact, a new feature was added to structure, code, stage and generate prescription orders based on the patient-clinician conversations. According to MobiHealthNews and Medium, the CEO and founder said that their AI Assistant had saved their clinicians up to 72% of documentation time by assisting with tasks, such as coding and answering questions.
In fact, AI scribes have been reported to potentially be a gamechanger in clinician workflows and reducing clinician workload – as shown in this YouTube video:
In Singapore, some of the AI scribes that are available include:
- Medow Health AI – Developed by an Australian healthtech company, this AI-powered scribe was deployed in over 500 clinics and hospitals in Australia, and expanded into Singapore. The platform has been adapted to local healthcare contexts, even supporting translations from Chinese, Cantonese, Malay and Indonesian.
- Hesyra – This chatbot app was developed as a healthtech project by our very own NUS pharmacy student (and I’m proud to have taught him before) 🙂 Am glad that he managed to get inspired by the NUS Overseas Colleges (NOC) program to get into the area of digital health! The app was tested in local clinics to transcribe doctor-patient conversations to clinical notes, and has since launched as a startup from Singapore!
- SgScribe – Currently in its beta phase, this AI-powered medical transcription app was developed locally and it transcribes consultations into SOAP notes (Subjective, Objective, Assessment, Plan) in 4 different languages (English, Chinese, Malay and Indonesian). Interestingly, the recordings are saved without any patient identifiers or personal details of patients.
- PlatoScribe – This AI clinical documentation tool is probably one of the oldest in Singapore, created by its parent company – Plato Medical. Integrated with its own ecosystem (known as Plato Clinic Management Software, or CMS), it is currently used by over 4,000 healthcare providers across Singapore, Australia and Asia-Pacific! This platform is one of the rate ones that is adapted to the local Singapore landscape, with multilingual support, compliance with the Personal Data Protection Act (PDPA), integration with Singpass, and also allows submission to the country’s National Electronic Health Record (NEHR).
- SingHealth’s Note Buddy – This in-house Gen AI system was built to summarize and transcribe patient-clinician consultations into clinical notes based on the 4 main languages in Singapore (English, Chinese, Malay and Tamil). Because it is built within a secure, internet-separated governmental platform by the country’s local healthtech agency, the consultation notes can be entered, stored, archived and accessed in a safe and efficient manner.
- AIGP Health’s Anzu – This agentic AI clinical assistant was developed by 4 doctors in Singapore. It also functions as a copilot that supports clinical judgment! Deployed via both WhatsApp and online, the AI assistant generates consultation notes that are “accurate, audit-compliant, and context-aware”, through structured history-taking, triaging and follow-up of patients.
- Open Government Products’ Scribe – Known as just “Scribe”, this transcription and summarization tool was created for public healthcare sectors access by GovTech. Catered for professions with heavy note-taking needs in mind, it documents the conversations as structured clinical notes, but with a twist – it can even support local accents and dialects, such as Singlish! Interestingly, the metrics provided as of 2025 Q3 states that it saves an average of up to 36.7 minutes per consultation and over 32,000 hours of total documentation time quarterly!
But with the hype of Gen AI right now, and the crowded AI scribe landscape, are we really there yet?
The Halo Effect in Digital Health
Before diving into the data, we need to address the elephant in the room: the Halo Effect surrounding AI scribes.
For those of you who don’t know what the Halo Effect is – it’s when one positive trait of a person influences the way others sees the person favorably, thus creating bias and/or clouding the judgment of that person’s character. Similar to the concept of seeing “halos” around angels, the bias is that by seeing someone with a “halo”, one may think that this person is a good person.
The same goes with digital health technologies… The Halo Effect exists when there is a positive impression of a feature or aspect of a product, service or company, which influences the overall judgment of the entire technology, or even other similar technologies like it.
The fact is that healthcare professionals are drowning in documentation. EPIC fatigue is real. Burnout rates have sky rocketed since the COVID-19 pandemic. So when a technology promises to “give clinicians their lives back” and “restore the joy of medicine,” the psychological appeal is overwhelming. As a healthcare professional myself, I truly understand how it feels to be “liberated” of these tedious tasks….
But here’s where there is a thin line between fact and reality:
- Do our perceptions of modest time savings feel more miraculous than it really is?
- We advocate data-driven decisions, but do anecdotal testimonials of health tech taint our decisions?
- Vendors know that they need an evidence base, so they collaborate to conduct studies on their health tech – but are the studies truly equivalent?
- Many vendors provide ROI projections based on small-scale studies. Are these real projections or wishful thinking on our part?
Sometimes, a good user interface (UI) and compelling demos can be more convincing than actual data. If something looks good, people tend to believe it will work better, even if it’s not true… The case of Gen AI hallucinations is an classic example.
But the Halo Effect is not unique to AI scribes – it has been a long-standing phenomenon, and has occurred repeatedly with digital health technologies. Given the scale of investment and the high stakes involved, do we really have the rigorous evidence needed to substantiate the benefits of ambient AI scribes?
Well, now we have it.
What the Evidence Shows from 2 RCTs
Study 1: University of Wisconsin (Afshar et al.1)
- Design: 66 healthcare practitioners randomized to Abridge vs control/usual care in three 6-week sequences of a 24-week stepped wedge RCT
- Setting: Multiple specialties, academic medical center with ambulatory clinics
- Result: ~22 minutes reduced per day, similar to human scribes; but burnout significantly improved without significant improvement in professional fulfilment
- Context: 71% physician uptake (essentially ideal conditions)
Study 2: University of California, Los Angeles – UCLA (Lukac et al.2)
- Design: 238 outpatient physicians across 14 specialties, three-arm pragmatic RCT for 2 months
- Interventions: Microsoft Dragon Ambient eXperience (DAX) Copilot vs Nabla vs control/usual care
- Results:
- Nabla: 9.5% reduction in time-in-note vs control (~7–12 minutes per session)
- DAX Copilot: No significant time savings vs control
- AI scribes saved less than a minute per visit (similar to other observational studies)
- Potential improvements in burnout, task load and work exhaustion (need confirmation in larger-scaled studies)
- Context: ~30% adoption rate across both (more reflective of real-world)
Four Critical Findings
1. Time Savings are Modest:
We are talking just minutes per day, not hours. Ambient AI scribes only saved ~7-12 mins per session, and in the best-case scenario – 22 minutes… Similar to human scribes. Is this really good enough for ROI for healthcare systems? The math doesn’t really work out for most specialties.
2. Burnout Reduction is Real:
At least in both trials, clinician burnout showed improvements across multiple measures:
- Work exhaustion (PFI-WE scores)
- Physician task load (PTL scores)
- Overall burnout (Mini-Z scores)
- Professional fulfilment (Stanford Professional Fulfillment Index) – non-significant increase
This is good news! With clinician burnout so rampant these days, any intervention that can reduce emotional fatigue and cognitive burden will have some inherent value, even if there are non-substantial gains.
3. Adoption Determines Impact:
The contrast between the Wisconsin (~71% uptake) and UCLA (~30% uptake) RCTs suggest that the adoption scale drastically affects results, and may not necessarily reflect real-world adoption and implementation. Some factors that may affect adoption include:
- Workflow integration complexity
- Patient consent processes
- Clinicians’ comfort with technology
- Organizational change management
Tech vendors that are selling their products based on best-case scenarios may be setting unrealistic expectations.
4. Ambient AI Scribes Are Still Just Assistants, Not Autopilots:
Although AI scribes show early promise of reducing clinician documentation, the UCLA trial identified clinically significant inaccuracies “occasionally” in both their AI scribes. There is still a need for “human-in-the-loop” – even for AI scribes. But even though we (as clinicians) always claim that AI hallucinations are bad, we must remember that we “humans” also make mistakes, and may not be able to comprehensively catch contradictions and inconsistencies. The moment when we (clinicians) become complacent about reviewing AI-generated content, we become fallible to medical errors – and instead of being a slice of cheese in the Swiss Cheese Model of incidents, we will unknowingly become the “holes”.

The Real Problem: We Are Only Fixing the Tip of the Iceberg
The accompanying editorial by Kim et al.3 makes a crucial point: ambient AI scribes only fixes the tip of the clinical workload iceberg.
Documentation is burdensome, yes. But clinicians spend massive amounts of time on:
- Reviewing results and reconciling data
- Following up on patient communications
- Writing orders and navigating order sets
- Authorizing for insurances
- Coding and billing
- Tracking down missing information
- Managing follow-up tasks
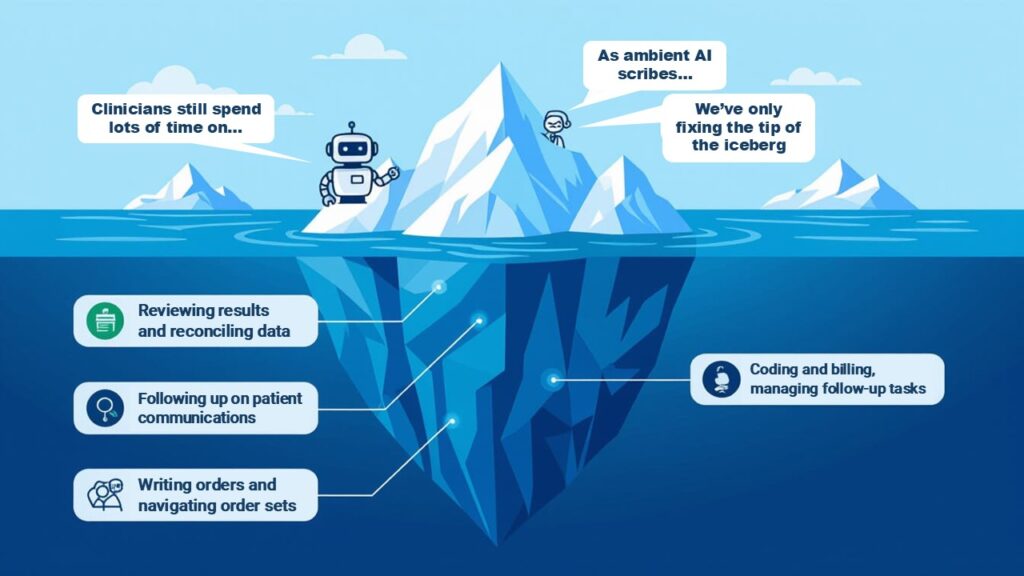
Although current AI scribes make note-taking easier, they cannot really do the above. The next generation of AI tools need to go beyond just passive translation and transcription to redesign clinical workflow processes, for example:
- Pre-visit chart synthesis
- Intelligent order entry
- Real-time prior authorization submission
- Automated follow-up task management
- Inbox triage and suggested responses
That’s when AI can become a true productivity tool, not just a wellness tool.
Food For Thought: Is Clinician Wellness Worth the Investment?
The evidence is clear from these 2 RCTs:
- ✅ AI scribes can reduce burnout (Should they be deployed for wellness?)
- ⚠️ Time savings are modest (Healthcare organizations that are expecting ROI may be having unrealistic expectations…)
- 🚀 Next generation of AI scribes will be transformative (if they can really tackle full clinical workflows, but we are not there yet…)
So what should the healthcare sector expect?
- For healthcare providers: Manage your expectations. Current AI scribes are just wellness tools that may help with clinician burnout, not productivity tools. Are we willing to sacrifice wellness for large scale productivity?
- For pharmacy sector: While technology exists, do we need specific pharmacy-built solutions that understand our unique workflows, safety requirements, and billing models? As part of Singapore’s National Pharmacy Strategy, the nation is embarking on a Next Generation Electronic Medical Record (NGEMR), National Billing System (NBS) and National Harmonised Integrated Pharmacy System (NHIPS). Will ambient AI scribes be able to be integrated in any of these systems in the future?
The future is not about replacing clinicians with AI. It is about liberating clinicians from their administrative burden, so that they can practice at the top of their license.
References:
- Afshar M, et al. A pragmatic randomized controlled trial of ambient artificial intelligence to improve health practitioner well-being. NEJM AI. 2025; 2(12). [DOI: 10.1056/AIoa2500945]
- Lukac PJ, et al. Ambient AI scribes in clinical practice: A randomized trial. NEJM AI 2025; 2(12). [DOI: 10.1056/AIoa2501000]
- Kim E, Liu VX, Singh K. AI scribes are not productivity tools (yet). NEJM AI 2025; 2(12). [DOI: 10.1056/AIe2501051]